Abstract
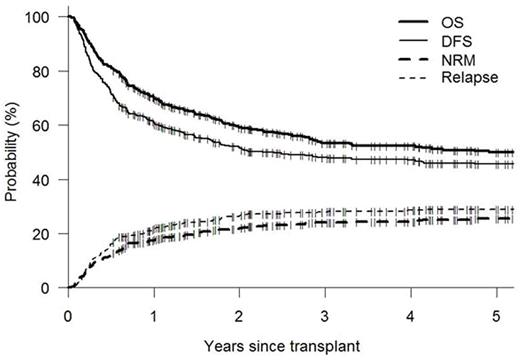
Patients undergoing allogeneic hematopoietic cell transplants (Allo-HCT) using myeloablative preparative regimens are usually admitted to an inpatient transplant unit from the start of the conditioning regimen until hematopoietic recovery (on average 25-35 days). Historically, the rationale for routine inpatient care during this period has been the facilitation of administration of parenteral medications, prevention of mold infections and the monitoring and management of acute toxicities. However, advances in supportive care and other technologies may allow outpatient management during this period. We analyzed outcomes of all consecutive patients who underwent myeloablative allo-HCT as defined by the CIBMTR (Giralt 2009, BBMT) with planned total outpatient management at our center. Patient characteristics and outcome data were prospectively entered into our institutional database from which they were extracted for this analysis. Patients were scheduled to receive their conditioning regimen and post-transplant care in our purpose-built outpatient clinic. Patients received their stem cell infusion on the inpatient unit and were planned to be discharged home the same day except patients receiving haploidentical transplants who were planned to be discharged on day +5 to accommodate the early cytokine release syndrome commonly seen in such patients (Solomon BBMT 2012). Subsequent admissions were for significant complications necessitating inpatient management only. Our technical approach to total outpatient management of myeloablative allo-HCT was as previously described (Solomon BMT 2010, 45: 468-475). Patients (n=462) were transplanted consecutively between 4/08 and 12/15. Patient characteristics were: median age 46; male (53%); race - white 79%, black 18%, Asian 2%; diagnosis- AML 42%, ALL 21%, MDS/MPS 21%, NHL/HL/CLL 13%, other 3%; donor type - MRD 48%, MUD 35%, Haplo 17%, CBT <1%; graft source- PBSC 87%, BM 12%, BM+PBSC 1%; regimen-busulfan based 60%, TBI based 39%, other 1%; DRI -low 16%, intermediate 48%, high 26%, v. high 10%; HCT-CI- 0-2 (64%), ≥3(36%). The conditioning regimen was entirely delivered in the outpatient clinic as planned in 377 patients (82%). Of 85 (18%) patients who received some of their conditioning regimen in the inpatient setting, in 42(49%) this was to receive drugs not administrable or reimbursed in the outpatient setting, and in 43(51%) it was for management of toxicity. The majority of patients were discharged within 24 hours of stem cell infusion (311 -67%) with the median day of discharge for the remaining patients being d+13 (range d+2 to d+75). Following discharge after stem cell infusion, 82 patients (18%) were never readmitted, days to readmission for the remainder were 0-5 (40%), 6-9 (24%), > 10 (18%). For readmitted patients, most frequent reasons were - febrile neutropenia 33%, mucositis 29%, and lower GI toxicity 4.5%. Median total length of inpatient stay through d+100 was 16 d (range 1-98). Fungal infections were documented in only 3 patients (1%) through d +100. With a median follow-up for surviving patients of 52 months (6-218 months), K-M estimates of survival and DFS at 1 yr are 70% and 61% and at 4 years are 52% and 47% respectively. Cumulative incidences (CI) of non-relapse mortality (NRM) and relapse at 1 yr are 17% and 21% and at 4 yrs are 24% and 29% (Fig.1). CI of acute GVHD grade 2-4 and 3-4 at 6 months were 28% and 10%. CI of moderate to severe, and severe chronic GVHD at 4 years were 30% and 12%. On multivariate analysis, receipt of any part of the conditioning regimen as inpatient was a significant negative factor for survival (HR 1.99, p<0.001), DFS (HR 1.74, p =0.001) and NRM (HR 2.06, p=0.004). These data show that myeloablative allo-HCT performed without routine inpatient admission from conditioning through neutrophil recovery is feasible with low rates of NRM and fungal infection. Median total inpatient stay through d +100 can be reduced to 16 days and nearly 20% of patients can avoid any inpatient stay through d +100. With mature follow-up outcomes appear similar or superior to those commonly reported using a traditional inpatient approach.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal