Abstract
In normal hematopoiesis, autophagy is essential for stem and progenitor cell (HSPC) function. We previously reported that basal autophagy is higher in HSPCs compared to more differentiated cells, and genetic interference with the autophagy machinery abolished in vivo engraftment of cord blood (CB) CD34+ cells (Stem Cells 2016).
To study the role of autophagy in acute myeloid leukemia (AML), steady-state autophagy was measured in a panel of myeloid leukemic cell lines (n=7) and primary human CD34+ AML cells (N=55). Autophagic flux was determined by the relative accumulation of cyto-ID (a marker for autophagic vesicles), measured by flow cytometry. Alternatively, autophagy was determined by LC3-II/p62 accumulation using Western blotting or fluorescence microscopy. Large variability in basal autophagy was observed in AML samples in contrast to CB CD34+ cells. Autophagic flux was significantly higher in AML CD34+ cells of patients belonging to poor-risk group (n=15) vs. intermediate and good-risk group (n=26, p=<0.001). Moreover, expression levels of the essential autophagy genes ATG5 and ATG7 were increased in AML CD34+ cells compared to normal bone marrow (NBM) CD34+ cells. Autophagy was functionally relevant for leukemic cells, because primary AML CD34+ cells (n=35) showed an increased susceptibility for the autophagy inhibitor hydroxychloroquine (HCQ), compared to NBM CD34+ cells (10µM HCQ, NBM CD34+: 84% ± 4 survival vs. AML CD34+: 43% ± 4, p=<0.001).
The blocking of autophagy by genetic interference (lentiviral shATG5 or shATG7) or by a pharmacological approach (HCQ) triggered an apoptotic response in leukemic cells,which coincided with increased expression of p53 and the downstream pro-apoptotic target genes BAX and PUMA, the putative AKT inhibitor PHLDA3 and the cell cycle inhibitor p21. This apoptotic phenotype could be rescued by the lentiviral shRNA mediated knockdown of p53. Interestingly, AMLs harboring TP53 mutations (TP53mut, N=6) did not respond to HCQ treatment compared to wild type P53 (P53wt) AMLs. In line, the pro-apoptotic BAX and PUMA expression was not upregulated upon HCQ treatment, suggesting that the apoptotic response was severely dampened in TP53mut AMLs. Co-treatment with Nutlin-3 (which stabilizes p53), enhanced the cytoxic effect of HCQ in P53wt AMLs, but not TP53mut AMLs. In contrast, overexpression of mutant p53R273H in the p53wt cell lines OciM3 and Molm13, rendered cells more resistant to HCQ treatment.
To further characterize autophagy in the leukemic stem cell (LSC) enriched cell fraction we separated AML CD34+ cellsin ROSlow and ROShigh cells, since previous studies have shown that LSCs are enriched in the ROSlow cell fraction. The CD34+ AML ROSlowcells had significantly lower mitochondrial mass and maintained a higher autophagy flux in comparison to the AML ROShigh cells (n=11, p=<0.05). In line, the autophagy regulator FOXO3A and the essential autophagy genes Beclin-1 and LC3 were expressed significantly higher in AML ROSlow cells. The increase in autophagy in AML ROSlowcells was also functionally relevant since these AML cells were more sensitive to HCQ treatment when compared with AML ROShigh cells. To validate the efficacy of autophagy inhibition in vivo, AML CD34+ cells of two different patients were transduced with the shATG5 or shSCR-GFP and subsequently transplanted in immunodeficient NSG mice. Inhibition of autophagy utilizing shATG5 prevented the in vivo engraftment of AML CD34+ cells in NSG mice.
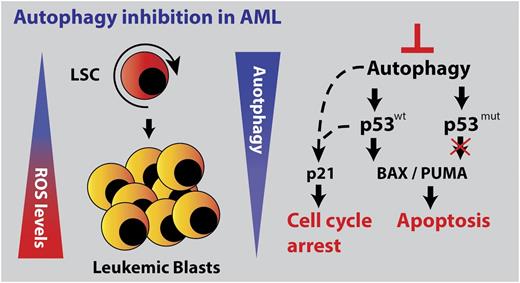
In conclusion, our results indicate that AML CD34+ cells are highly dependent on the autophagy machinery for growth and cell survival, in a p53-dependent manner. Targeting autophagy, potentially in conjunction with conventional chemotherapeutics might provide new therapeutic options for treatment of P53wt AMLs (Figure 1).
Model, left part: LSCs are enriched in the ROS low fraction of AML blasts. ROS low cells maintain a higher basal autophagy flux compared ROS high cells. Right part: Genetic or pharmacological inhibition of autophagy triggered a p53 dependent apoptotic response in p53 wild type AMLs, which is severely dampened in TP53 mutant AMLs.
Model, left part: LSCs are enriched in the ROS low fraction of AML blasts. ROS low cells maintain a higher basal autophagy flux compared ROS high cells. Right part: Genetic or pharmacological inhibition of autophagy triggered a p53 dependent apoptotic response in p53 wild type AMLs, which is severely dampened in TP53 mutant AMLs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal