Key Points
Neutrophils can present cognate antigens to antigen-specific memory CD4+ T cells.
MHC-II and costimulatory molecules are induced on neutrophils in the presence of antigen and antigen-specific memory CD4+ T cells.
Abstract
Neutrophils are critical cells of the innate immune system and rapidly respond to tissue injury and infection. Increasing evidence also indicates that neutrophils have versatile functions in contributing to adaptive immunity by internalizing and transporting antigen and influencing antigen-specific responses. Here, we demonstrate that freshly isolated human neutrophils can function as antigen-presenting cells (APCs) to memory CD4+ T cells. Neutrophils pulsed with the cognate antigens cytomegalovirus pp65 or influenza hemagglutinin were able to present the antigens to autologous antigen-specific CD4+ T cells in a major histocompatibility complex class II (MHC-II; HLA-DR)-dependent manner. Although myeloid dendritic cells and monocytes showed superior presenting ability, neutrophils consistently displayed antigen presentation capability. Upregulation of HLA-DR on neutrophils required the presence of the antigen-specific or activated T cells whereas exposure to innate stimuli such as Toll-like receptor ligands was not sufficient. Neutrophils sorted from vaccine-draining lymph nodes from rhesus macaques also showed expression of HLA-DR and were capable of presenting vaccine antigen to autologous antigen-specific memory CD4+ T cells ex vivo. Altogether, the data demonstrate that neutrophils can adapt a function as APCs and, in combination with their abundance in the immune system, may have a significant role in regulating antigen-specific T-cell responses.
Introduction
Neutrophils are the most abundant circulating leukocytes and are critical effector cells of the innate immune system.1-3 They express a wide range of pattern recognition receptors, including Toll-like receptors (TLRs),4 Fc receptors, and complement components,5 and they have the capacity to kill microorganisms through a combination of phagocytosis, release of cytotoxic granules, and use of neutrophil extracellular traps.6,7 Following infection or trauma, neutrophils rapidly migrate to inflamed tissues. Neutrophils infiltrating sites of inflammation, like those containing an infection or tissue damage or those induced by vaccine administration, internalize antigen and may subsequently migrate to draining lymph nodes (dLNs).8,9 Studies in mice and sheep have shown that neutrophils are the first cells to transport phagocytosed antigen in afferent lymph vessels after vaccination.8,10,11 Antigen-positive neutrophils are found both in lymph nodes (LNs) and spleen, particularly under inflammatory conditions like infections and sterile inflammation.10,12-16 The migration of neutrophils to lymphoid organs both in humans and mice has been linked to upregulation of the chemokine receptor CCR7 and consequently is impaired in CCR7−/− mice.17
Along with reaching lymphoid organs, it has been proposed that neutrophils contribute to adaptive immune responses by transporting and presenting antigen and regulating antigen-specific responses.18-21 Both at the site of inflammation as well as in LNs, neutrophils have been shown to interact with lymphocytes and antigen-presenting cells (APCs) or may act as APCs themselves.22,23 Surface expression of markers associated with antigen presentation capacity, like major histocompatibility complex class II (MHC-II) and costimulatory molecules, can be induced in human neutrophils by exposure to granulocyte-macrophage colony-stimulating factor (GM-CSF), interferon γ (IFN-γ,), interleukin 3 (IL-3), and tumor necrosis factor (TNF), resulting in their ability to present antigens, for example, tetanus toxoid or Staphylococcus aureus superantigens, to CD4+ T cells.24-26 Interestingly, neutrophils from patients with autoimmune disorders such as active Wegener granulomatosis27,28 and rheumatoid arthritis29 show elevated surface expression of MHC-II, CD80, and CD86 compared with healthy controls. This was also observed in a mouse model of chronic colitis where neutrophils transported antigens to inflamed gut and acted as APCs.30 Furthermore, murine bone marrow–derived neutrophils exposed to GM-CSF acquired a neutrophil–dendritic cell (DC) hybrid phenotype exhibiting DC markers and APC functionality, while retaining neutrophil properties.31
There is, therefore, emerging evidence that neutrophils are versatile cells that contribute to generating and/or maintaining antigen-specific T-cell responses to a much greater extent than previously thought. In the current study, we compared human neutrophils with classical APCs, that is, DCs and monocytes to determine their antigen presentation capacity. In addition, we explored the conditions required to induce APC function, including the expression of MHC-II and costimulatory molecules. In order to study neutrophils in vivo, we used a nonhuman primate (NHP) model expressing a high degree of similarities with human counterparts to confirm that antigen-positive neutrophils in dLNs are capable of presenting antigen.
Materials and methods
A detailed description and additional methods are available in supplemental Methods (available on the Blood Web site).
Donor consent
The study was performed in accordance with the Helsinki declaration and approved by the institutional review board of ethics at the Karolinska Institutet, Stockholm, Sweden. Blood was collected from healthy human individuals after informed consent.
Isolation of human peripheral blood neutrophils by Polymorphprep
Human neutrophils were isolated from fresh peripheral blood using Polymorphprep (Axis-Shield) centrifugation (purity ≥85%). Cells were resuspended in RPMI 1640 (Sigma-Aldrich) with 100 U/mL penicillin, 100 μg/mL streptomycin, 292 μg/mL l-glutamine (Hyclone), and 10% fetal bovine serum (Gibco) for experimentation or in phosphate-buffered saline (PBS) plus 2% fetal bovine serum for further purification by flow cytometry sorting.
Isolation of human APC subsets by flow cytometry sorting
CD66abce+ neutrophils were purified using a FACSJazz cell sorter (BD Biosciences) from the Polymorphprep-enriched neutrophils. Where indicated, neutrophils, monocytes, and DC subsets were simultaneously purified from the monocyte-sized cell fraction collected by automated apheresis, followed by elutriation and finally sorting using a panel of specific markers (supplemental Table 1) by a FACSAria flow cytometer (BD Biosciences) (purity ≥99%).
Antigen presentation assay in vitro
Freshly purified neutrophils, monocytes, and DCs from donors with detectable cytomegalovirus (CMV) pp65-specific and/or influenza hemagglutinin (HA)-specific CD4+ T-cell recall responses were pulsed at 37°C for 1 hour with recombinant pp65 (5 μg; Miltenyi Biotec) or HA (5 μg; Novartis). The cells were cocultured with autologous CD4+ T cells isolated by the RosetteSep CD4+ T-cell enrichment kit (StemCell Technologies) and labeled with carboxyfluorescein diacetate succinimidyl ester (CFSE; Molecular Probes) at an APC-to-T-cell ratio of 1:10.32,33 After 5 days, CD4+ T-cell proliferation was evaluated by flow cytometry (see supplemental Methods).
Immunization of NHPs and sample processing
Indian rhesus macaques were housed at Bioqual (Rockville, MD), and handled according to the standards of the Association for Assessment and Accreditation of Laboratory Animal Care. Animals received intramuscular immunizations at 0, 4, 12, and 24 weeks with recombinant HIV-1 envelope glycoprotein (Env) (100 μg, TV-1 strain; Novartis) in adjuvant. Blood was collected and peripheral blood mononuclear cells were isolated using Ficoll (GE Healthcare) as previously described33 and stored at −80°C until used. A final boost with an Alexa Fluor 680–labeled HIV-1 Env (AF680-Env; 100 μg) was given 1.5 years later when the Env-specific T-cell response had waned. One arm received AF680-Env while the contralateral arm received PBS as control. dLNs from both sides and the spleen were collected after 24 hours and processed directly by gentle mechanical mincing to obtain single-cell suspensions. For antigen uptake studies, muscle biopsies from the injection sites were processed and analyzed for vaccine-positive cells as described earlier (see supplemental Methods).34
Antigen presentation assay ex vivo
AF680-Env+ neutrophils and myeloid DCs (MDCs) were sorted from the LNs draining the Env-administered arm using FACSAria according to the gating strategy described in Figure 6A. Neutrophils and MDCs sorted from the distal PBS-draining LNs served as controls. CD4+ T cells were sorted using a FACSAria from stored peripheral blood mononuclear cells collected at the peak time point for T-cell responses (2 weeks after the fourth immunization). Neutrophils and MDCs were cocultured with CFSE-labeled autologous CD4+ T cells for 5 days to evaluate T-cell proliferation as described in the previous section. In parallel, neutrophils, monocytes, and MDCs were sorted by flow cytometry from the spleen, and pulsed in vitro for 1 hour with Env (2 µg) before adding autologous CFSE-labeled CD4+ T cells (see supplemental Methods). Antibodies are listed in supplemental Table 1.
Statistical analysis
Data were analyzed using Prism 6.0 (GraphPad Software) and presented as mean ± standard error of the mean (SEM) of at least 3 independent experiments. The unpaired Student t test or 2-way analysis of variance were used for comparison between 2 or multiple groups. A P value < .05 was considered statistically significant.
Results
Isolation and phenotypic characterization of human neutrophils
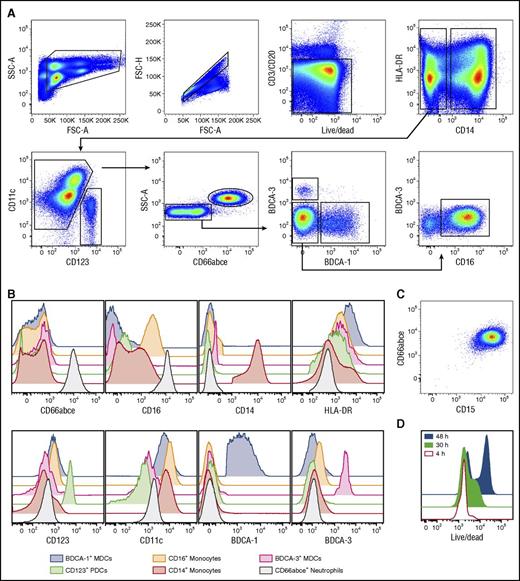
In order to isolate and functionally compare different APC populations, we developed a multicolor staining panel for flow cytometry–based isolation of neutrophils, CD14+ and CD14−CD16+ monocytes, and DC subsets (Figure 1A). The isolated populations were phenotyped for their differential expression of CD66abce, CD16, CD14, HLA-DR, CD123, CD11c, BDCA-1, and BDCA-3 (Figure 1B). As expected, isolated neutrophils expressed CD66abce and CD16 plus low levels of CD11c but not CD14 or the DC-associated markers BDCA-1 and BDCA-3. We verified that CD66abce+ neutrophils coexpressed CD15 (Figure 1C). In addition, neutrophils expressed no or very little HLA-DR.
Simultaneous isolation of pure populations of human neutrophils, monocytes, and DC subsets by flow cytometry cell sorting. (A) Pure populations of human CD66abce+ neutrophils, CD14+ and CD14−CD16+ monocytes, CD123+ PDCs, and CD11c+ MDC subsets (BDCA-1+ and BDCA-3+ subsets) were isolated from the elutriated monocyte-fraction after apheresis by flow cytometry sorting according to the depicted gating strategy. CD14−CD16+ monocytes are now indicated as CD16+ monocytes only for simplicity. (B) Representative flow histograms show the expression levels of the indicated markers on the sorted APC populations. (C) Sorted CD66abce+ neutrophils coexpress CD15. (D) Representative flow histograms show the live/dead staining (LIVE/DEAD fixable dead cell stain kit) on sorted neutrophils over time. Neutrophils showed high viability for at least 30 hours and can be maintained in culture longer. A representative donor of 6 is shown. FSC-A, forward scatter area; FSC-H, forward scatter height; SSC-A, side scatter area.
Simultaneous isolation of pure populations of human neutrophils, monocytes, and DC subsets by flow cytometry cell sorting. (A) Pure populations of human CD66abce+ neutrophils, CD14+ and CD14−CD16+ monocytes, CD123+ PDCs, and CD11c+ MDC subsets (BDCA-1+ and BDCA-3+ subsets) were isolated from the elutriated monocyte-fraction after apheresis by flow cytometry sorting according to the depicted gating strategy. CD14−CD16+ monocytes are now indicated as CD16+ monocytes only for simplicity. (B) Representative flow histograms show the expression levels of the indicated markers on the sorted APC populations. (C) Sorted CD66abce+ neutrophils coexpress CD15. (D) Representative flow histograms show the live/dead staining (LIVE/DEAD fixable dead cell stain kit) on sorted neutrophils over time. Neutrophils showed high viability for at least 30 hours and can be maintained in culture longer. A representative donor of 6 is shown. FSC-A, forward scatter area; FSC-H, forward scatter height; SSC-A, side scatter area.
Recent findings indicate that the lifespan of neutrophils is not as short as previously thought.35,36 We monitored the cell viability of neutrophils by using a live/dead dye at 4, 30, and 48 hours of culture post–flow cytometry sorting. Neutrophils showed similar viability to fresh cells for at least 30 hours whereas increased cell death was evident at 48 hours (Figure 1D). Similar results were observed in neutrophils isolated by the Polymorphprep procedure which offered more rapid isolation of highly enriched neutrophils (≥85%) with larger cell yields as compared with flow sorting. Neutrophil viability was again well maintained for 30 hours (supplemental Figure 1A-B).
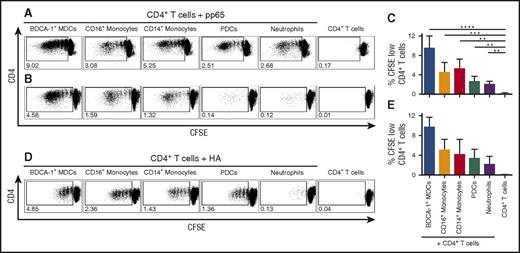
Neutrophils can present cognate antigens to antigen-specific memory CD4+ T cells in vitro at a low but consistent level
We earlier developed a method to evaluate antigen presentation based on presentation of the cognate CMV pp65 antigen for which detectable memory T-cell responses are common in healthy CMV-seropositive blood donors.37-39 We used this method to assess whether neutrophils are capable of presenting antigens to T cells in a side-by-side comparison with monocyte and DC subsets. Flow cytometry–sorted neutrophils and monocyte and DC subsets were incubated with pp65 and cocultured with CFSE-labeled autologous CD4+ T cells for 5 days. The efficiency of the different populations to present pp65 to pp65-specific T cells was evaluated by the degree of responding proliferating T cells. BDCA-1+ MDCs showed a clearly superior antigen presentation capacity as evidenced by the higher levels of proliferating CD4+ T cells (Figure 2A-C). CD16+ and CD14+ monocytes showed somewhat lower capacity although they were also potent at inducing T-cell proliferation. Plasmacytoid DCs (PDCs) and neutrophils showed a markedly lower but consistent ability to present antigen to CD4+ T cells and induce proliferation (Figure 2A-C). Due to limited cell yields, BDCA-3+ MDCs were not included in the comparison. The same pattern was observed with an alternative antigen, HA, in donors with detectable HA-specific T-cell responses (Figure 2D-E). Neutrophil viability in the neutrophil-T-cell cocultures was similar as compared with neutrophils cultured alone (supplemental Figure 1C-D).
Neutrophils can present antigens to antigen-specific memory CD4+T cells but MDCs and monocytes have the highest capacity. Sorted APCs from CMV- or influenza-seropositive donors were pulsed respectively with CMV pp65 or influenza HA and cocultured with autologous CFSE-labeled CD4+ T cells. Their capacity to present antigen to CD4+ T cells was evaluated by measuring proliferating T cells (CFSE dilution). (A,B,D) Proliferating (CFSE low) CD4+ T cells in presence of the indicated APCs from 2 CMV-seropositive donors (A-B) or 1 representative HA-seropositive donor (D) are shown. Bars show percentages of (C) pp65-specific and (E) HA-specific proliferating CD4+ T cells (mean ± SEM, n = 6 and n ≥ 2 healthy human donors, respectively). **P < .01, *** P < .001, **** P < .0001.
Neutrophils can present antigens to antigen-specific memory CD4+T cells but MDCs and monocytes have the highest capacity. Sorted APCs from CMV- or influenza-seropositive donors were pulsed respectively with CMV pp65 or influenza HA and cocultured with autologous CFSE-labeled CD4+ T cells. Their capacity to present antigen to CD4+ T cells was evaluated by measuring proliferating T cells (CFSE dilution). (A,B,D) Proliferating (CFSE low) CD4+ T cells in presence of the indicated APCs from 2 CMV-seropositive donors (A-B) or 1 representative HA-seropositive donor (D) are shown. Bars show percentages of (C) pp65-specific and (E) HA-specific proliferating CD4+ T cells (mean ± SEM, n = 6 and n ≥ 2 healthy human donors, respectively). **P < .01, *** P < .001, **** P < .0001.
To validate the finding that neutrophils can function as APCs to antigen-specific memory CD4+ T cells, a series of control experiments was performed. First, we confirmed that the level of T-cell proliferation was minimal when CD4+ T cells were cultured alone with antigen or together with neutrophils but without the antigen (Figure 3A-B). This was in contrast to the low but persistent level of T-cell proliferation observed in the donor-matched cultures of neutrophils, antigen, and T cells (Figure 3A-B). Furthermore, we found that the T-cell proliferation induced by neutrophils was mediated by HLA-DR as it was strongly reduced in the presence of a neutralizing antibody to HLA-DR. In contrast, no reduction was observed in the presence of an isotype control antibody (Figure 3C).
Human neutrophils present the antigen to antigen-specific memory CD4+T cells in an HLA-DR–dependent manner. Neutrophils from CMV- or influenza-seropositive donors were pulsed with pp65 or HA and cocultured with autologous CFSE-labeled CD4+ T cells for 5 days. (A) Representative plots of HA (where indicated) or pp65-specific proliferating CD4+ T cells for the indicated conditions. (B-C) Bars show percentages of pp65-specific proliferating CD4+ T cells. (C) HLA-DR neutralizing antibody strongly reduced CD4+ T-cell proliferation mediated by neutrophils whereas no reduction was observed in presence of the same concentration of isotype control (mean ± SEM, n = 3-8 donors); *P < .05, **P < .01 and #P < .01 vs CD4+ T cells only. (D) CD4+ T-cell proliferation induced by neutrophils alone or in presence of different amounts of BDCA-1+ MDCs (up to 10%) or CD14+ monocytes (up to 10%).
Human neutrophils present the antigen to antigen-specific memory CD4+T cells in an HLA-DR–dependent manner. Neutrophils from CMV- or influenza-seropositive donors were pulsed with pp65 or HA and cocultured with autologous CFSE-labeled CD4+ T cells for 5 days. (A) Representative plots of HA (where indicated) or pp65-specific proliferating CD4+ T cells for the indicated conditions. (B-C) Bars show percentages of pp65-specific proliferating CD4+ T cells. (C) HLA-DR neutralizing antibody strongly reduced CD4+ T-cell proliferation mediated by neutrophils whereas no reduction was observed in presence of the same concentration of isotype control (mean ± SEM, n = 3-8 donors); *P < .05, **P < .01 and #P < .01 vs CD4+ T cells only. (D) CD4+ T-cell proliferation induced by neutrophils alone or in presence of different amounts of BDCA-1+ MDCs (up to 10%) or CD14+ monocytes (up to 10%).
Although much effort in this study was focused on refining isolation methods for highly pure neutrophils, a potential risk is that the sorted populations may contain contaminating APCs that could potentially induce T-cell activation, resulting in misleading results. We therefore evaluated how many bona fide professional APCs, such as BDCA-1+ MDCs or CD14+ monocytes, are needed to induce significantly higher T-cell proliferation over that induced by neutrophils alone. Increasing levels of sorted BDCA-1+ MDCs or CD14+ monocytes were added to the sorted neutrophils. The cell mix was cocultured with T cells and proliferation was measured as for the antigen presentation assay. We found that >1% of contaminating BDCA-1+ MDCs or >10% of contaminating monocytes were needed in the neutrophil population to result in significantly increased T-cell proliferation (Figure 3D). Because neutrophils isolated by flow cytometry sorting were about 99% pure and the contaminating cells represented a mix of cells, it is unlikely that the key observation that neutrophils can present antigen to T cells stems from contaminating DCs or monocytes. Finally, we verified that antigen presentation capacity was a mutual function among low- or normal-density neutrophils which indicates that this is not only related to a specific subset (supplemental Figure 2).
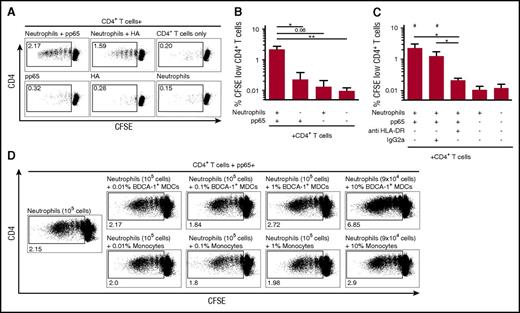
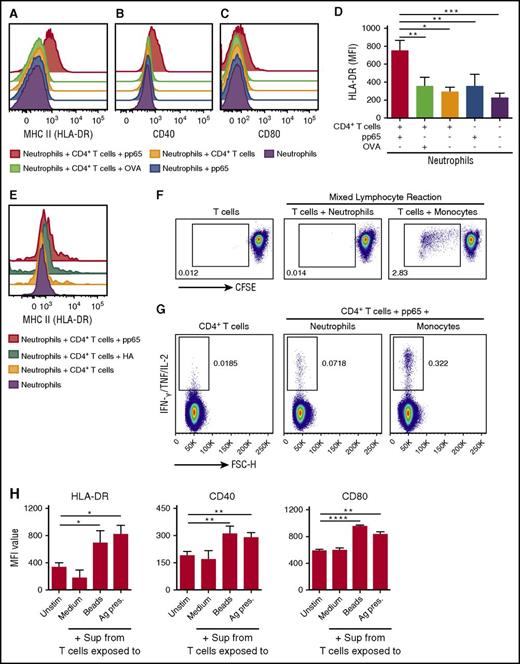
Induction of MHC-II and costimulatory molecules on neutrophils requires interaction with antigen-specific CD4+ T cells
Freshly isolated neutrophils expressed no or very little MHC-II or any of the costimulatory molecules CD86, CD80, CD40, and CD83. Because these receptors are critical for antigen presentation, we addressed what stimuli are required for their induction in neutrophils. Using cells from CMV-seropositive donors, we found that coincubation of neutrophils with autologous CD4+ T cells and pp65 resulted in marked levels of MHC-II (HLA-DR) as well as detectable CD80 and CD40 (Figure 4A-D). In contrast, no HLA-DR expression was observed on neutrophils that had been cocultured with CD4+ T cells without antigen or neutrophils exposed to pp65 alone. Similar results were observed for HA and T cells from donors with detectable HA-specific T-cell responses (Figure 4E). We did not detect HLA-DR upregulation on neutrophils cultured with autologous CD4+ T cells and ovalbumin to which no memory T-cell responses existed in the donor (Figure 4A,D) or when the cells were sorted from CMV-seronegative donors with no detectable response to pp65 (not shown). This suggests that both the antigen and responding antigen-specific CD4+ T cells are required for induction of MHC-II on neutrophils. Consistent with this, we found that HLA-DR expression on unstimulated neutrophils was insufficient to drive a mixed lymphocyte reaction of naive T cells (Figure 4F). Apart from induction of T-cell proliferation, neutrophils also induced cytokine production (IFN-γ, IL2, and/or TNF) in pp65-specific memory T cells, again at a lower level compared with classical APCs like monocytes (Figure 4G). IFN-γ has been shown to stimulate HLA-DR on neutrophils.40 In support of this, we found that fresh neutrophils exposed to supernatants from T cells, activated either by anti-CD3/CD28 beads or by neutrophils presenting antigen, upregulated expression of HLA-DR and the costimulatory molecules CD40 and CD80 (Figure 4H) as well as CD83 and CD11b (supplemental Figure 3A).
Upregulation of MHC-II (HLA-DR), CD40, and CD80 on neutrophils requires antigen and antigen-specific memory CD4+T cells. Representative histograms show the surface expression levels of HLA-DR (MHC II) (A,E) and the maturation markers CD40 (B) and CD80 (C) on neutrophils cultured for 30 hours alone or with autologous CD4+ T cells for all the indicated conditions. (D) Bar graphs show geometric mean fluorescence intensity (MFI) values of HLA-DR (mean ± SEM, n = 4 donors). (F) Proliferation of allogeneic naive T cells in a mixed lymphocyte reaction induced by neutrophils or monocytes. One representative donor of 3 is shown. (G) IFN-γ/IL-2/TNF production in responding pp65-specific CD4+ T cells stimulated by neutrophils or CD14+ monocytes. One representative donor of 3 is shown. (H) Bar graphs show the surface expression levels of HLA-DR, CD40, and CD80 on neutrophils after stimulation for 30 hours with supernatants (Sup) collected from culture of T cells only (Medium), T cells activated with anti-CD2/CD3/CD28 beads (Beads), or from the neutrophil–T-cell cocultures prepared as for the Ag presentation assay (Ag pres) (mean ± SEM, n = 4). *P< .05, **P < .01, ***P < .001, ****P < .0001. Unstim, unstimulated.
Upregulation of MHC-II (HLA-DR), CD40, and CD80 on neutrophils requires antigen and antigen-specific memory CD4+T cells. Representative histograms show the surface expression levels of HLA-DR (MHC II) (A,E) and the maturation markers CD40 (B) and CD80 (C) on neutrophils cultured for 30 hours alone or with autologous CD4+ T cells for all the indicated conditions. (D) Bar graphs show geometric mean fluorescence intensity (MFI) values of HLA-DR (mean ± SEM, n = 4 donors). (F) Proliferation of allogeneic naive T cells in a mixed lymphocyte reaction induced by neutrophils or monocytes. One representative donor of 3 is shown. (G) IFN-γ/IL-2/TNF production in responding pp65-specific CD4+ T cells stimulated by neutrophils or CD14+ monocytes. One representative donor of 3 is shown. (H) Bar graphs show the surface expression levels of HLA-DR, CD40, and CD80 on neutrophils after stimulation for 30 hours with supernatants (Sup) collected from culture of T cells only (Medium), T cells activated with anti-CD2/CD3/CD28 beads (Beads), or from the neutrophil–T-cell cocultures prepared as for the Ag presentation assay (Ag pres) (mean ± SEM, n = 4). *P< .05, **P < .01, ***P < .001, ****P < .0001. Unstim, unstimulated.
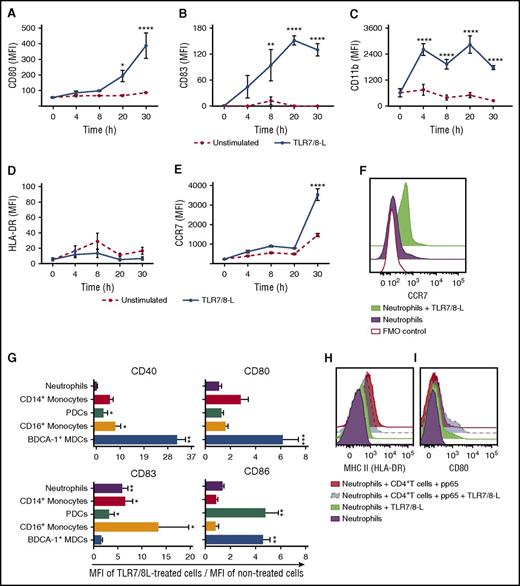
Neutrophil exposure to TLR ligands induces costimulatory molecules but not MHC-II
To further address the requirements for induction of a phenotype on neutrophils associated with antigen-presenting capacity, we exposed the cells to a TLR7/8-L. TLR7/8-L is known to transform DCs and monocytes into a mature phenotype.37,41 As neutrophils have been shown to express functional TLR8 but not TLR7,42 we measured neutrophil activation after exposure to TLR7/8-L over time by analyzing the levels of CD80, CD83 as well as CD11b and CCR7. We found that neutrophil activation was rapid and robust in response to TLR7/8-L (Figure 5A-F). Increased levels of CD83 and CD11b were already observed after 4 hours and the cells maintained the phenotype for 30 hours, again supporting that neutrophils can be functional over a continuous period of time. Upregulation of CD80 and CCR7 was detected at 20 to 30 hours. However, TLR7/8-L was not sufficient for HLA-DR upregulation on neutrophils (Figure 5D,H; supplemental Figure 3B). Consistent with this, the TLR ligands lipopolysaccharide and flagellin did not upregulate HLA-DR either, despite evidence of activation found by upregulation of CD83 and CD11b (supplemental Figure 3C-F).
TLR7/8-L induces neutrophil activation but is not sufficient for the induction of MHC-II molecules. (A-F) Neutrophils exposed to TLR7/8-L were phenotypically characterized over time by flow cytometry. TLR7/8-L activated neutrophils as detected by upregulation of CD80 (A) and CD83 (B) as well as upregulation of the integrin CD11b (C) over time but was not sufficient for the upregulation of HLA-DR (D). TLR7/8-L enhanced CCR7 levels on neutrophils (E-F). Quantified MFIs of the indicated markers ± SEM on neutrophils over time (A-E) and representative histograms of the surface expression levels of CCR7 from a representative donor of 3 at 30 hours (F) are shown. (G) Surface expression levels of CD80, CD86, CD40, and CD83 on distinct sorted APCs after overnight exposure to TLR7/8-L. Data are presented as ratio of the MFI values between TLR7/8-L–treated and unstimulated cells ± SEM. (H-I) Representative histograms show the surface expression levels of HLA-DR (H) and CD80 (I) on human neutrophils cultured for 30 hours alone or in presence of autologous CD4+ T cells and pp65 with or without TLR7/8-L (2.5 μg/mL); n = 3-5 healthy human donors. *P < .05, **P < .01, ***P < .001, ****P < .0001. FMO, fluorescence minus one.
TLR7/8-L induces neutrophil activation but is not sufficient for the induction of MHC-II molecules. (A-F) Neutrophils exposed to TLR7/8-L were phenotypically characterized over time by flow cytometry. TLR7/8-L activated neutrophils as detected by upregulation of CD80 (A) and CD83 (B) as well as upregulation of the integrin CD11b (C) over time but was not sufficient for the upregulation of HLA-DR (D). TLR7/8-L enhanced CCR7 levels on neutrophils (E-F). Quantified MFIs of the indicated markers ± SEM on neutrophils over time (A-E) and representative histograms of the surface expression levels of CCR7 from a representative donor of 3 at 30 hours (F) are shown. (G) Surface expression levels of CD80, CD86, CD40, and CD83 on distinct sorted APCs after overnight exposure to TLR7/8-L. Data are presented as ratio of the MFI values between TLR7/8-L–treated and unstimulated cells ± SEM. (H-I) Representative histograms show the surface expression levels of HLA-DR (H) and CD80 (I) on human neutrophils cultured for 30 hours alone or in presence of autologous CD4+ T cells and pp65 with or without TLR7/8-L (2.5 μg/mL); n = 3-5 healthy human donors. *P < .05, **P < .01, ***P < .001, ****P < .0001. FMO, fluorescence minus one.
A head-to-head functional comparison between donor-matched neutrophils, monocytes, and DC subsets with regard to their phenotypic maturation to TLR7/8-L was also performed (Figure 5G). As expected, DCs and monocytes responded strongly to TLR7/8-L. Neutrophils did not upregulate costimulatory molecules to the same high levels.
Because HLA-DR expression on neutrophils appeared to be more tightly regulated than the expression of costimulatory molecules, we investigated whether TLR7/8-L exposure would amplify HLA-DR expression when added in the presence of T cells. Neutrophils were exposed to TLR7/8-L alone or in the presence of pp65 and CD4+ T cells from CMV-seropositive donors to evaluate their degree of activation. Again, TLR7/8-L alone was not sufficient to induce HLA-DR, nor did it further increase the levels of HLA-DR on neutrophils induced by coculture with pp65 and CD4+ T cells (Figure 5H). In contrast, in presence of TLR7/8-L, higher levels of CD80 were observed (Figure 5I). We therefore concluded that although neutrophils respond to TLR7/8-L, they require both an antigen and antigen-specific T cells or exposure to cytokines secreted by activated T cells to express detectable levels of HLA-DR. The presence of pathogen-associated signals such as TLR ligands may not be enough to transform neutrophils into functional APCs. Importantly, even under conditions where neutrophils interact with antigen-specific T cells, the expression of HLA-DR induced on neutrophils is much lower compared with the levels on classical APCs such as monocytes and DCs. Therefore, their ability to present antigens and activate T cells will likely never reach the efficiency of professional APCs.
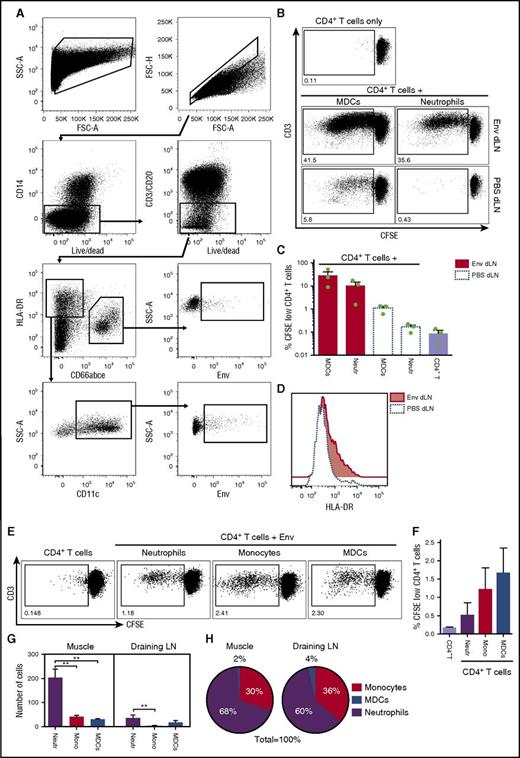
Neutrophils from vaccine-draining LNs are capable of antigen presentation
The presence of antigen-positive neutrophils in lymphoid organs of vaccinated animals is well documented.8,11,43 To approach antigen presentation capacity of neutrophils in vivo, we studied neutrophils and DCs in dLNs of vaccinated rhesus macaques. As there is great similarity in the cell-specific receptors expressed on neutrophils and DCs between rhesus macaques and humans, this model is powerful for providing evidence of antigen presentation capacity of neutrophils in vivo. For the studies, we used animals that had been previously immunized with the vaccine candidate HIV-1 Env glycoprotein and developed detectable Env-specific CD4+ T-cell responses. For the purpose of this study, the animals were boosted again with an AF680-Env so that we could visualize and isolate Env+ neutrophils from the dLNs at 24 hours after administration. LNs draining the opposite arm receiving PBS served as a control. Neutrophils and MDCs were isolated by flow cytometry sorting (Figure 6A) and cocultured with autologous CFSE-labeled CD4+ T cells to again evaluate T-cell proliferation. In line with the in vitro data, the ex vivo–isolated neutrophils were found to present antigen to antigen-specific memory CD4+ T cells at a low but consistent level. Neutrophils isolated from the Env-draining LNs induced well-detectable T-cell proliferation but MDCs showed the highest capacity (Figure 6B-C). Neutrophils sorted from the PBS-draining LNs did not induce T-cell proliferation, indicating that the observed responses were Env-specific. MDCs sorted from the PBS-draining LNs showed higher background proliferation but much lower than that induced by the counterparts isolated from the Env-draining LNs. We observed that the neutrophils sorted from the Env-draining LNs showed markedly higher HLA-DR levels than the neutrophils sorted from the PBS-draining LNs (Figure 6D).
Neutrophils sorted from the dLNs after vaccination present Env to memory CD4+T cells but MDCs have the highest capacity. (A) Neutrophils and MDCs were isolated by flow cytometry sorting from the dLNs of vaccinated rhesus macaques 24 hours postinjection with an Alexa 680–labeled Env or PBS (contralateral arm) according to the depicted gating strategy. (B) Neutrophils isolated from the Env-draining LNs induced well-detectable T-cell proliferation but MDCs showed the highest capacity. Representative plots of proliferating CD4+ T cells. (C) Bars graph show percentages of proliferating CD4+ T cells (mean ± SEM, n = 3 NHPs). (D) Representative histograms show HLA-DR levels on neutrophils sorted from the Env and PBS dLNs. (E) Representative plots show proliferating CD4+ T cells after 5-day cocultures with either neutrophils, monocytes, or MDCs isolated from spleen from the animals above in presence of Env. (F) Bars show percentages of proliferating CD4+ T cells (mean ± SEM, n = 3 NHPs). (G-H) Rhesus macaques were injected with Alexa 680–labeled Env and the cell subsets recruited to the muscle injection site and dLNs were phenotyped and enumerated by flow cytometry. (G) Number of indicated cell subsets mobilized to the Env-injected muscle and dLNs (mean ± SEM, n = 3 NHPs); **P < .01. (H) Proportions of the number of Env+ cell subsets at the injection site and draining LNs. Mono, monocytes; Neutr, neutrophils.
Neutrophils sorted from the dLNs after vaccination present Env to memory CD4+T cells but MDCs have the highest capacity. (A) Neutrophils and MDCs were isolated by flow cytometry sorting from the dLNs of vaccinated rhesus macaques 24 hours postinjection with an Alexa 680–labeled Env or PBS (contralateral arm) according to the depicted gating strategy. (B) Neutrophils isolated from the Env-draining LNs induced well-detectable T-cell proliferation but MDCs showed the highest capacity. Representative plots of proliferating CD4+ T cells. (C) Bars graph show percentages of proliferating CD4+ T cells (mean ± SEM, n = 3 NHPs). (D) Representative histograms show HLA-DR levels on neutrophils sorted from the Env and PBS dLNs. (E) Representative plots show proliferating CD4+ T cells after 5-day cocultures with either neutrophils, monocytes, or MDCs isolated from spleen from the animals above in presence of Env. (F) Bars show percentages of proliferating CD4+ T cells (mean ± SEM, n = 3 NHPs). (G-H) Rhesus macaques were injected with Alexa 680–labeled Env and the cell subsets recruited to the muscle injection site and dLNs were phenotyped and enumerated by flow cytometry. (G) Number of indicated cell subsets mobilized to the Env-injected muscle and dLNs (mean ± SEM, n = 3 NHPs); **P < .01. (H) Proportions of the number of Env+ cell subsets at the injection site and draining LNs. Mono, monocytes; Neutr, neutrophils.
To confirm that neutrophils from another lymphoid organ also can present antigens, we sorted neutrophils, monocytes, and MDCs from the spleen of the same animals. The cells were pulsed with exogenous Env. Neutrophils were again found to induce Env-specific CD4+ T-cell proliferation but at a lower level than monocytes and MDCs (Figure 6E-F). To evaluate the proportions of neutrophils vs other APCs that internalized antigen, we compared the levels of Env+ cell populations at the injection site in the muscle and in dLNs 24 hours after AF680-Env administration. Neutrophils were the largest population that was mobilized to Env-injected muscle and dLNs (Figure 6G). Consequently, neutrophils were proportionally the most common Env+ cell type (Figure 6H). The abundance of antigen-positive neutrophils in vivo could therefore potentially make up for some of their low antigen-presenting capacity compared with professional APCs.
Discussion
Neutrophils were long thought to be short-lived cells of the innate immune system. However, there is increasing evidence that they can survive for several days and that under several conditions they can acquire classical APC markers and functions.21,40 Previous studies have described neutrophil trafficking to lymphoid organs22,44 and their antigen uptake ability.11 It has also been proposed that neutrophils can serve as APCs or influence the capacity of professional APCs to present antigens.11,45 For example, DCs can take up antigens acquired from phagocytosed apoptotic neutrophils.46
In the current study, we investigated whether neutrophils are viable for a sufficient time and can acquire antigen presentation capacity to contribute to adaptive immunity. We found that neutrophils are able to present cognate antigens to autologous memory CD4+ T cells in vitro and ex vivo although to a lower extent compared with MDCs and monocytes. Neutrophils isolated from blood of healthy donors expressed no or very little MHC-II and costimulatory molecules that are required for antigen presentation. They therefore need to undergo a phenotypic transformation in order to acquire APC abilities. Although our data showed that TLR ligands could induce costimulatory molecules on freshly sorted neutrophils in culture, upregulation of MHC-II required the presence of both antigen and the antigen-specific memory CD4+ T cells or alternatively supernatant from activated T cells secreting IFN-γ and other cytokines. This is in contrast to professional APCs such as MDCs that persistently express detectable levels of these molecules and readily acquire a mature phenotype after exposure to a variety of stimuli such as TLR ligands. Even under the conditions that did lead to upregulation of costimulatory molecules and HLA-DR on neutrophils, substantially lower expression levels were found on neutrophils compared with MDCs and monocytes. Neutrophils may therefore not be able to prime naive CD4+ T cells as indicated by their inability to induce allogeneic naive T-cell activation. However, neutrophils suffice presentation to memory T cells that have lesser requirement of high MHC and costimulatory marker expression.
Neutrophils express MHC-II and costimulatory molecules after exposure to specific cytokines like GM-CSF, IFN-γ, and IL-3,24,25,40 suggesting that under specific environmental conditions neutrophils can acquire APC phenotype and functions without requiring antigen-specific memory CD4+ T cells. This can be of particular significance for patients treated with IFN-γ or GM-CSF commonly used in the treatment of cancer or chronic infectious diseases.47 Neutrophils have been shown to play an important role in transporting antigen to lymphatic compartments.11,43,48 In line with this, we found readily detectable antigen-positive neutrophils at the muscle injection site and in LNs draining this site in the arm of rhesus macaques. When the neutrophils were sorted and cultured with autologous T cells they showed that they could present and activate antigen-specific memory CD4+ T cells. The data again reflect antigen presentation to already primed memory T cells and the ability of neutrophils to prime naive T cells still remains elusive.
In our study, antigen-positive neutrophils sorted from the vaccine-draining LNs showed higher expression of HLA-DR compared with neutrophils isolated from the PBS-draining LNs. This mimics the in vitro finding and suggests that neutrophils require both the antigen and antigen-specific T cells in order to upregulate MHC-II in vivo or alternatively be in a milieu where activated T cells secrete cytokines as a consequence of responding to antigen presentation by proximal APCs. The capacity to degrade and load antigens to MHC-II is essential for a cell to function as an APC. The amount of antigen delivered to the processing compartment strongly affects the antigen presentation. Professional APCs such as DCs have proteases and peptide-receptive MHC molecules at their cell surface and are able to present antigens by direct binding at the cell surface in addition to antigen processing by intracellular proteases.49 In contrast, neutrophils express MHC-II and costimulatory molecules on their surface only after appropriate stimulation and even if they are efficient at collecting antigens, the endosomal processing of antigens for MHC presentation may be a limiting step as shown for macrophages.50,51 Neutrophils, as macrophages, are key cells for the clearance of invading microorganisms. Their lysosomal compartments may be better adapted for digestion of internalized materials, resulting in fast antigen degradation and limited antigen processing.52,53 The generation of appropriate peptides for binding to MHC molecules is crucial and requires limited proteolytic processing.
It appears that neutrophils have a much more important role in adaptive immune responses than previously thought. The ability of neutrophils to present antigens may play a pathogenic role in autoimmune conditions where these cells are present at sites of inflammation in patients with rheumatoid arthritis and Wegener granulomatosis.27-29 Moreover, tumor-infiltrating neutrophils have been observed in different human cancers54 where they transport tumor antigens from tumor sites to lymphoid tissues to induce immune responses.55 Multiple neutrophil phenotypes, in particular in cancer and inflammation, have been described.56,57 This heterogeneity likely explains the different roles played by neutrophils in different environmental conditions.58,59 In contrast to support T-cell responses, neutrophils have also been reported to have strong suppressive effects on adaptive immune responses in a mouse model.60 Neutrophil infiltration led to reduced DC-to-T-cell interactions and inhibited T-cell egress from the LNs by producing thromboxane A2.60 In the latter case, neutrophils may affect the amount of available antigen by phagocytosis, and thus limit antigen presentation by professional APCs. Our in vivo findings suggest that MDCs and monocytes may be deprived from antigens to some extent due to the concurrent mobilization of numerous neutrophils with high antigen uptake ability to the site of antigen delivery. MDCs and neutrophils are at the opposite ends of antigen presentation; MDCs are rare but excel in T-cell stimulation, and neutrophils are frequent but inefficient at inducing T-cell responses. Collectively, the data presented here demonstrate that neutrophils can function as APCs both in vitro and in vivo. Further experiments in DC-deficient individuals or using equivalent mouse models would help to clarify whether neutrophils can make up for the lack of professional APCs including priming and regulation of adaptive immunity.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank David Ambrozak for help with cell sorting by flow cytometry and J.-P. Todd and the animal care personnel at Bioqual. The authors also thank Susan Barnett and Derek O’Hagan, GSK Vaccine (formerly Novartis), for providing the vaccine antigens for immunization.
This work was supported by a grant from the Swedish Medical Council (Vetenskapsrådet) (K.L.). M.V. was supported by a grant from the Foundation Blanceflor Boncompagni-Ludovisi, the Swedish Society of Medicine, and the Fernström Foundation. A.L. was supported by a grant from the China Scholarship Council and a PhD salary grant from Karolinska Institutet. This article is also based upon work from the European Cooperation in Science and Technology (COST) Action BM1404 European Network of Investigators Triggering Exploratory Research on Myeloid Regulatory Cells (www.mye-euniter.eu), supported by COST. COST is part of the European Union Framework Program Horizon 2020.
Authorship
Contribution: M.V., A.L., A.N.-T., R.A.K., F.L., and K.L. designed research; M.V., A.L., and F.L. performed and analyzed experiments; and M.V., A.L. and K.L. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Karin Loré, Immunology and Allergy Unit, Department of Medicine, Karolinska Institutet, 171 76 Stockholm, Sweden; e-mail: karin.lore@ki.se.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal