To the editor:
KIR3DL2, a killer immunoglobulin-like receptor normally expressed by a subset of natural killer (NK) cells, is aberrantly expressed in Sézary syndrome (SS), an aggressive cutaneous T-cell lymphoma (CTCL). In SS patients, the detection of KIR3DL2 expression on circulating tumor cells using flow cytometry is useful for diagnosis, follow-up of circulating tumor cell burden, and prognosis.1,2 The detection of KIR3DL2, PLS3, Twist, and NKp46 gene expression in the blood using reverse transcription polymerase chain reaction (RT-PCR) may also be used for reliable SS diagnosis.3 KIR3DL2 expression has been demonstrated in skin biopsy samples from 10 SS and 10 transformed mycosis fungoides (tMF) patients using RT-PCR and immunohistochemistry (IHC) and 11 primary cutaneous anaplastic large cell lymphoma (cALCL) samples using flow cytometry, RT-PCR, and IHC.4-6
Recently, KIR3DL2-targeted therapy and the development of IPH4102, a monoclonal antibody directed against KIR3DL2 that demonstrated in vitro and in vivo antitumor activity in preclinical studies, have raised hope for SS treatment.7 IPH4102 appears to be safe and have beneficial clinical activity in the IPH4102-101 phase 1 study (NCT02593045).8
In a context of unmet medical need for therapy of patients with advanced-stage CTCL, we studied the expression of KIR3DL2, the IPH4102 target, in all CTCL World Health Organization subtypes9 to identify all potential candidates for KIR3DL2-targeted therapy. The secondary objectives were to study the association between KIR3DL2 in situ expression and mycosis fungoides (MF)/SS disease stage and examine the potential prognostic value of KIR3DL2 in situ expression for overall survival (OS) in CTCL.
In 134 CTCL patients who provided informed consent, frozen skin biopsy samples were evaluated using immunohistochemistry with the KIR3DL2-specific MOG1-MK323-12B11 monoclonal antibody.6 This clone does not cross-react with KIR3DL1, unlike the AZ158 clone used in previous studies.4,5 The investigations were performed in accordance with the Declaration of Helsinki and French law. KIR3DL2 expression was assessed independently by 2 pathologists and expressed as the median percentage of KIR3DL2-positive lymphoid cells in 10 high-power fields. Results in CTCL patients were compared with 10 erythrodermic inflammatory disease (EID) patients and 10 healthy donors. Median KIR3DL2 expression in EID was chosen as a cutoff value for analysis of CTCL cases. Clinical data of CTCL patients (age, sex, International Society for Cutaneous Lymphomas European Organisation for Research and Treatment of Cancer disease stage at biopsy,10,11 extracutaneous involvement, and OS from biopsy) were collected (supplemental Table 1, available on the Blood Web site). The Mann-Whitney U test was used to compare KIR3DL2 expression between patient groups, and the Kruskal-Wallis test was used to analyze KIR3DL2 expression through MF/SS disease stages (Prism software version 7; GraphPad, La Jolla, CA). Interobserver agreement was studied using a κ test (GraphPad). For prognostic analysis of OS, univariate and multivariate analyses were performed using the Cox proportional hazard regression model (MedCalc software version 17.4; MedCalc, Ostend, Belgium). Factors with P < .20 in univariate analysis were included for multivariate analysis.
The study cohort included 48 MF patients (including 6 folliculotropic and 2 granulomatous slack skin variant cases), 25 tMF patients, 21 SS patients, 12 cALCL patients, 6 lymphomatoid papulosis patients, 6 HTLV1 adult T-cell lymphoma patients, 4 extranodal NK/T-cell lymphoma patients, 3 γδ T-cell lymphoma patients, 3 peripheral T-cell lymphoma not otherwise specified patients, 2 subcutaneous panniculitis-like T-cell lymphoma patients, 2 CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma patients, and 2 small-to-medium CD4-positive lymphoproliferative disease (LPD) patients.
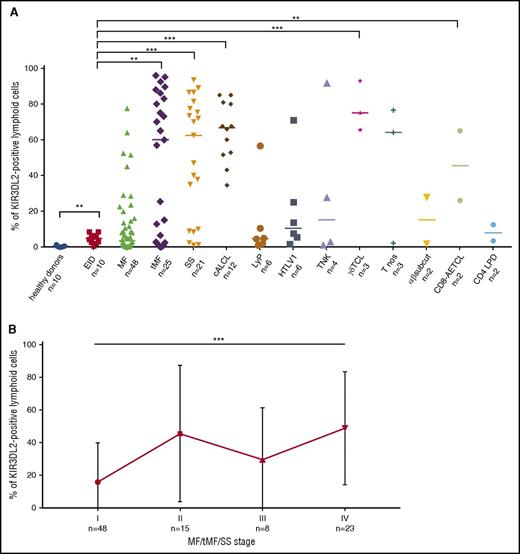
Interobserver agreement for KIR3LD2 expression evaluation on frozen IHC stainings was very good (κ = 0.94). A median of 0.2% (range, 0% to 1.3%) and 4.85% (range, 0.5% to 8.5%) of cells were positive for KIR3DL2 in healthy donor skin and inflammatory infiltrate of EID skin samples, respectively. In all CTCL categories, >5% of lymphoid cells were KIR3DL2 positive in 88 out of 134 (65.7%) patients (Figure 1A; supplemental Figure 1). High expression (>50% KIR3DL2-positive lymphoid cells) was found in 48 (35.8%) patients when including all CTCL categories except HTLV1 adult T-cell lymphoma, CD4-positive LPD, and subcutaneous panniculitis-like T-cell lymphoma. KIR3DL2 was significantly more expressed in tMF, SS, cALCL, γδ T-cell lymphoma, and CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma patients than in EID patients (Figure 1A). Because our KIR3DL2 detection technique is limited to frozen samples, it may not be readily available in all laboratories. Therefore, the development of KIR3DL2 messenger RNA in situ hybridization on formalin-fixed paraffin-embedded samples may be of interest.
KIR3DL2 expression in CTCL. (A) KIR3DL2 expression in CTCL subtypes compared with healthy donors and EID patients (MF, including 2 granulomatous slack skin and 6 folliculotropic MF cases). αβ subcut, subcutaneous panniculitis-like αβ T-cell lymphoma; γδTCL, cutaneous γδ T-cell lymphoma; CD8-AETCL, CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma; HTLV1, HTLV1 adult T-cell lymphoma; LyP, lymphomatoid papulosis; TNK, T/NK nasal-type lymphoma; T nos, cutaneous peripheral T-cell lymphoma not otherwise specified. (B) KIR3DL2 expression according to International Society for Cutaneous Lymphomas European Organisation for Research and Treatment of Cancer disease stage in MF, tMF, and SS patients. **P < .01; ***P < .001.
KIR3DL2 expression in CTCL. (A) KIR3DL2 expression in CTCL subtypes compared with healthy donors and EID patients (MF, including 2 granulomatous slack skin and 6 folliculotropic MF cases). αβ subcut, subcutaneous panniculitis-like αβ T-cell lymphoma; γδTCL, cutaneous γδ T-cell lymphoma; CD8-AETCL, CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma; HTLV1, HTLV1 adult T-cell lymphoma; LyP, lymphomatoid papulosis; TNK, T/NK nasal-type lymphoma; T nos, cutaneous peripheral T-cell lymphoma not otherwise specified. (B) KIR3DL2 expression according to International Society for Cutaneous Lymphomas European Organisation for Research and Treatment of Cancer disease stage in MF, tMF, and SS patients. **P < .01; ***P < .001.
In the 94 patients with MF/SS, the median percentage of KIR3DL2-expressing lymphoid cells increased with disease stage (P = .0004; Figure 1B). Of the 94 MF/SS patients analyzed, >5% lymphoid cells were KIR3DL2 positive in 57 patients (61%). Expression of KIR3DL2 increased with stage (>5% of cells were KIR3DL2 positive in 46% of stage I patients [22 out of 48], 67% of stage II patients [10 out of 15], 75% of stage III patients [6 out of 8], and 83% of stage IV patients [19 out of 23]). KIR3DL2 was also significantly more expressed in MF/SS cases with large cell transformation, a known prognostic marker of worse survival,12 than in cases without large cell transformation (P = .0003). These results indicate that KIR3DL2 expression is present not only in advanced MF/SS but also in a subset of early MF cases. These findings also confirm that high KIR3DL2 expression is a characteristic feature of tMF and SS patients. Among the 73 MF/tMF patients, 6 out of 8 erythrodermic T4-stage patients had >5% KIR3DL2-positive cells, and 1 out of 2 patients with secondary blood involvement (B1 stage) had >50% KIR3DL2-positive cells. Among the 21 SS patients, a highly positive correlation was found between KIR3DL2 expression in the skin sample and peripheral blood (r = 0.821; Pearson correlation test).
The prognostic value of KIR3DL2 expression has previously been demonstrated in the circulating tumor cells of SS patients, and high KIR3DL2 expression was associated with shorter survival.1 In our entire CTCL cohort of 134 patients, multivariate Cox regression analysis revealed that age >60 years, the presence of extracutaneous involvement (N or M), and KIR3DL2 expression in >10% of skin lymphoid cells were independently associated with shorter OS (P = .02, P = .0007, and P = .02, respectively, in multivariate analysis), whereas male sex was not (P = .38). In the 94 patients with MF/SS, the factors independently associated with shorter OS in multivariate analysis included male sex, stage IIB or higher, and large-cell transformation (P = .02, P = .04, and P < .0001, respectively), but not age >60 years or KIR3DL2 expression >10% of skin lymphoid cells (P = .08 and P = .26, respectively). The number of non-MF/SS CTCL patients in our study precluded multivariate analysis of OS factors in this subgroup. Overall, the prognostic value of KIR3DL2 expression in >10% of skin lymphoid cells was detected in the entire cohort but requires further prospective investigation, especially in patients with non-MF/SS CTCL.
Altogether, these results identified significant KIR3DL2 expression in all CTCL subtypes, thus expanding the number of candidates for KIR3DL2-targeted therapy. In future clinical studies of IPH4102, patients with all CTCL subtypes should therefore be included. Translational studies of KIR3DL2 involvement in noncutaneous peripheral T-cell lymphomas will also be required to examine whether patients with nonprimary CTCL could benefit from KIR3DL2-targeted therapy. It will also be necessary to assess prospectively whether the clinical effect of IPH4102 is related to the percentage of KIR3DL2 expressing lymphoid cells to optimize the treatment of advanced CTCL.
The online version of this article contains a data supplement.
Authorship
Acknowledgments: The authors thank Angela Swaine-Verdier for editing the manuscript.
This study was supported in part by research funding from INSERM, Innate Pharma, and Université Paris 7 (M. Battistella, A.B., M. Bagot, and A.J.).
Contribution: M. Battistella and A.J. designed the study, performed research, analyzed data, and wrote the paper; C.L. and C.R.-W. performed research and reviewed the paper; C.H. and C.B. analyzed data and reviewed the paper; M. Bagot designed the study and reviewed the paper; H.S. and A.B. reviewed the paper. M. Battistella and A.J. had full access to all of the data in the study and take full responsibility for the integrity of the data and the accuracy of the data analysis; and all authors discussed and interpreted the results, vouch for the accuracy of the data, and collaborated in the preparation of the manuscript.
Conflict-of-interest disclosure: M. Battistella has a consulting/advisory role at Innate Pharma, receives honoraria from Bristol-Myers-Squibb, receives research funding from Innate Pharma; C.B. and H.S. are employed by Innate Pharma and own stock in Innate Pharma; A.B. and M. Bagot are coinventors of the patent entitled “means for the diagnosis and therapy of CTCL” licensed by INSERM to Innate Pharma, receive research funding from Innate Pharma, and own stock in Innate Pharma; and A.J. receives research funding from Innate Pharma. The remaining authors declare no competing financial interests.
Correspondence: Maxime Battistella, Pathology Department, Hôpital Saint Louis APHP, 1 Ave Claude Vellefaux, 75010 Paris, France; e-mail: maxime.battistella@aphp.fr.
References
Author notes
M. Bagot and A.J. contributed equally to this study.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal