Abstract

Introduction: In diffuse large B-cell lymphoma (DLBCL), hemoglobin (Hb) at diagnosis is often low. In other cancers, pre-therapeutic anemia has been identified as an independent predictor of poor outcome and incorporated in well-established prognostic indices. The aim of our study was to investigate whether this also could apply to DLBCL.
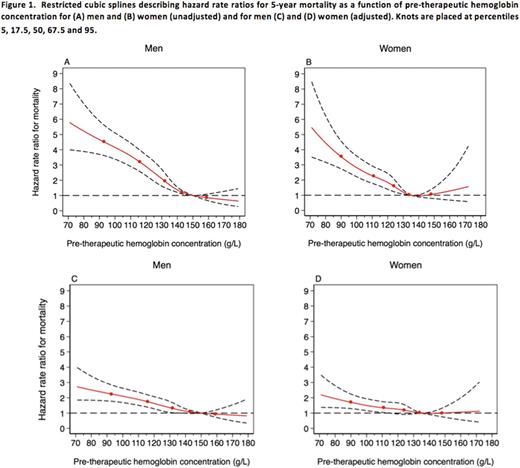
Methods:Clinical and laboratory data from DLBCL patients diagnosed between 2000 and 2012 were retrieved from nation-wide registries. Inclusion criteria were: a confirmed diagnosis of de novo DLBCL, treatment with anthracycline-containing chemotherapy with or without rituximab and no primary CNS-lymphoma. Four subgroups of pre-treatment Hb values (g/L) were defined for men/women: (i) >149/>133, (ii) 134-149/118-133, (iii) 98-133/98-117 and (iv) <98. While subgroup i and ii represented normal Hb levels either over or under the mean value for healthy individuals, subgroups iii and iv defined increasing grades of anemia. Correlation analyses between Hb subgroups and the clinical parameters contained in the National Comprehensive Cancer Network-International Prognostic Index (NCCN-IPI), sex, comorbidity and rituximab treatment were performed. Five-year overall (OS) and progression free survival (PFS) were estimated according to the method of Kaplan and Meier. A uni- and multivariable Cox regression model was used to calculate 5-year hazard rate ratios (HRR) for death or disease progression depending on Hb subgroup (where subgroup i was used as reference), NCCN-IPI, sex, comorbidity, and rituximab treatment with mutual adjustment. Finally, restricted cubic splines, stratified on sex, were used to illustrate the relative risk for death as a function of Hb at diagnosis.
Results:In total, 3,531 patients fulfilled the inclusion criteria. Hb levels below normal (subgroup iii and iv), were found in 1,612 patients (46%). Notably, pre-therapeutic anemia was more frequent in men (53%) than in women (38%). Anemia was correlated with elevated lactate dehydrogenase, disseminated disease and involvement of extranodal sites such as bone marrow, gastrointestinal tract, lung or liver. Patients with a normal Hb, but below the median value for healthy individuals had inferior outcome with a HRR for death of 1.55 (95% confidence interval [95%CI] 1.29-1.88). In subgroups iii and iv the HRR was 2.79 (95%CI 2.34-3.31) and 4.56 (95% CI 3.70-5.61). After adjusting for NCCN-IPI, sex, comorbidity and rituximab treatment, the HRR remained significantly increased for Hb subgroups ii, iii and iv, compared with subgroup i (reference). Patients treated with rituximab had a significantly better OS in all Hb subgroups and an adjusted HRR of 0.62 (0.55-0.70). When progression free survival was used as end point similar results were obtained. The restricted cubic splines illustrated the inverse correlation between Hb at diagnosis and the risk of death over a subsequent five-year period (Figure 1).
Conclusion:In this nationwide cohort study, anemia at diagnosis was a strong and independent predictor of both overall and progression free survival. This finding persisted after adjusting for NCCN-IPI score, sex, treatment with rituximab and comorbidity. The importance of Hb for prognosis was further evidenced by the fact that even a lowering of Hb within the range of normal (subgroup ii), resulted in an increased risk of death.
Clausen: Takeda: Research Funding. Nørgaard: Program for Clinical Research Infrastructure (PROCRIN): Research Funding. d'Amore: Les Laboratoires Servier: Honoraria, Other: Advisory Board; Nordic Nanovector: Other: Advisory Board; Sanofi: Research Funding; Takeda Pharma: Honoraria, Other: Advisory Board, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal