Abstract
Introduction: In classical Hodgkin lymphoma (cHL), new agents are initially investigated after several relapses in pre-treated patients. Evidence regarding disease status, treatment sequence, and survival after 3rd or higher relapse of cHL is limited. The aim of this study was to describe clinical outcomes of a historical group of European patients from the German Hodgkin Study Group (GHSG) trial database.
Methods: Subjects with at least three consecutive tumor-related events, either progressive/refractory or relapsed disease, were identified in the GHSG database. Two sub-cohorts, further analyzed, included patients (pts) suffering from 3rd relapse after autologous stem-cell transplantation (ASCT; cohort A); and 3rd relapse after salvage therapy without ASCT (cohort B). Overall survival (OS) was the main and progression free survival (PFS) a key secondary endpoint of this study. Adverse events (AEs) were collected in case they had been reported by treating physicians.
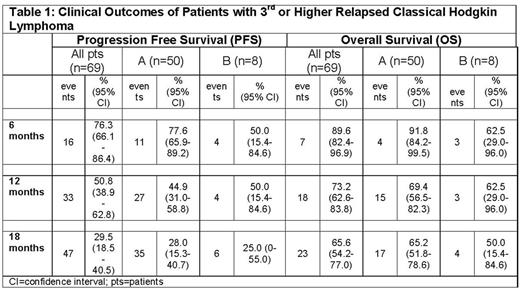
Results: More than 12,000 HL patients were identified from the GHSG database between the years 1993 and 2013; of which a total of 69 cHL patients with 3 or more relapsed/refractory disease events were included in the analysis. (A, N=50; B, N=8). Majority were males (n=51; 74%). Mean age at the time of 3rd relapse was 39.2 years (standard deviation = 14.0 years; range from 20 to 79 years), with the majority presenting with stage III or IV disease (67%). Time from end of 3rd-line treatment to 3rd relapse was ≤ 3 months (i.e. GHSG definition of refractory disease) in 15 pts (22%), ≤ 12 months (early relapse) in 19 pts (28%) and > 12 months (late relapse) in 35 pts (51%). All 69 pts were pretreated with chemotherapy (ctx), 35 pts (50.7%) with BEACOPP, 30 pts (43.5%) with ABVD and no BEACOPP, and 32 pts (46.4%) with other types of ctx. The number of prior ctx ranged from one to three (median 3). Pretreatment with radiotherapy was observed in 57 pts (82.6%), with salvage ctx aimed to induce a remission prior to stem-cell transplantation (SCT) in 58 pts (84.1%), and with high-dose ctx followed by ASCT in 50 pts (72.5%). Four pts (5.8%) had received allogeneic SCT as 3rd-line treatment. None of the pts had received brentuximab vedotin or anti-PD1 antibodies before 3rd relapse. Among 18 pts with AE records, 16 had a therapy-related AE >/= grade 3. Of the total 69 pts, objective response was obtained in 22 pts (31.9%, 95% CI 21%-44%). With a median observation time of 63.3 months for OS after 3rd relapse, 45 pts (65%) had died and 60 pts (87%) had another PFS event. Twelve months after the 3rd relapse, OS was 73.2% (95% CI 62.6%-83.8%; A, 69.4 % [95% CI 56.5%-82.4%]; B, 62.5 % [95% CI 29.0%-96.0%];) and PFS 50.8% (95%>CI 38.9% to 62.8%; A, 44.9 % [95% CI 31.0%-58.8%]; B, 50.0 % [95% CI 15.4%-84.6%]; Table 1).
Conclusion: Pts with a 3rd relapse or progression of cHL were young (mean age 39.2 years) and had poor clinical outcomes. More than 50% of the pts had a PFS event and a quarter of the patient population died within a year. The present data helps to further elucidate the patient-relevant value of new treatment options in a European health service context, and beyond and warrants the need for new treatment options to improve outcomes for these heavily affected pts.
Broeckelmann: Takeda: Consultancy, Honoraria, Research Funding; BMS: Honoraria, Research Funding. Kaskel: MSD; Merck & Co., Inc.: Employment, Other: stock/stock options. Metterlein: MSD: Employment. Giezek: MSD: Employment. Balakumaran: Merck & Co., Inc.: Employment, Other: stock/stock options. Raut: Merck & Co., Inc.: Employment, Other: stock/stock options. Engert: Amgen: Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Affimed: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding. von Tresckow: MSD: Consultancy, Research Funding; Takeda: Consultancy, Other: Travel, Housing, Congress Fees, Research Funding; Novartis: Honoraria, Other: Travel, Housing, Congress Fees, Research Funding; BMS: Other: Travel, Housing, Congress Fees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal