Abstract
Introduction: Antibody-mediated thrombotic thrombocytopenic purpura (TTP) is a rare disease with significant morbidity and mortality, requiring prompt diagnosis and intervention. The advent of rituximab use (off-label) for TTP in 2002 not only established a novel therapy for refractory disease, but also raised the possibility of prophylactic therapy. Prophylactic rituximab was found by Westwood et al. to be effective in normalizing ADAMTS13 when activity dropped ≤15% in a retrospective cohort study (Blood Advances, 2017). Treatment paradigms in TTP are changing as evidence builds for prophylactic therapy, but we remain without large, randomized data to guide who would benefit most from prophylactic rituximab.
The use of a rapid assay for a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13) has been shown to significantly reduce therapeutic plasma exchange (TPE) by ruling-in or -out suspected cases of TTP (Connell et al., Transfusion 2016). The role of rapid ADAMTS13 testing in assessment of response to TPE in acute TTP as well as surveillance of TTP patients in remission continues to be explored. We describe the utilization of a rapid ADAMTS13 assay and its role in the decision to use early or prophylactic rituximab in patients with TTP at the largest referral center for TTP in Rhode Island.
Methods: Following IRB approval, demographic data for patients who underwent rapid ADAMTS13 testing from 1/1/13-2/28/17 at Rhode Island Hospital (Providence, RI) was obtained. Patients were deemed to have TTP if they had thrombocytopenia with microangiopathic hemolytic anemia (MAHA) and ADAMTS13 ≤ 10%, or thrombocytopenia with MAHA and a history of TTP. Each patient admission for TTP was recorded as a separate event. Data analysis was performed using Wilcoxon rank sum and Fisher's exact tests.
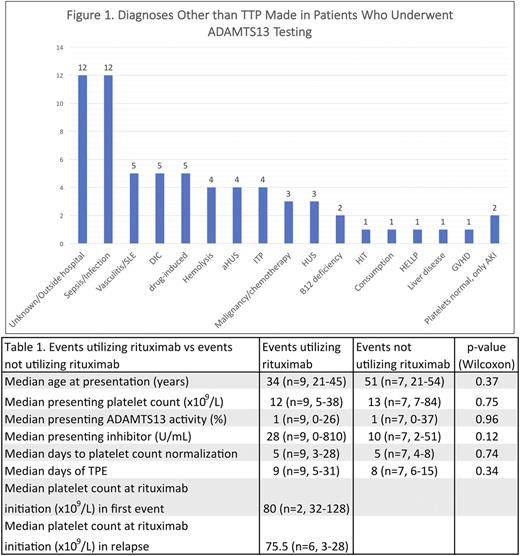
Results: Ninety patients had ADAMTS13 testing from 1/1/13 to 2/28/17. Seven patients were excluded due to age less than 18 years. The remaining 83 patient charts were reviewed. Sixteen events of acquired TTP were diagnosed in 11 patients. Pregnancy-associated TTP did not occur, although 1 relapse of TTP had a history of post-partum TTP. Of the remaining patients, 5 had a history of TTP and underwent surveillance testing of ADAMTS13. One patient had congenital TTP. Diagnoses other than TTP were characterized in 66 patients (Figure 1). The most common other diagnosis found in patients who underwent ADAMTS13 testing was sepsis (n=12).
When comparing patients who received rituximab during acute event (n=9) to those that did not (n=7) in 16 TTP events, we observed no statistically significant correlation between rituximab use and age, sex, presenting platelet count, presenting ADAMTS13 activity, presenting ADAMTS13 inhibitor value, days to platelet count normalization, or days of TPE (Table 1). We also observed no significant difference in days of TPE or days to platelet count normalization when comparing patients who received rituximab ≤ 5 days of diagnosis (n=5) versus those who received rituximab > 5 days from diagnosis but during the event (n=4). There was no significant change in rapid ADAMTS13 activity assay use, TPE use or rituximab use by year, from 2013-2016.
In three patients with a history of acquired TTP, routine follow-up ADAMTS13 activity assay revealed decreased activity prior to the development of thrombocytopenia. These patients had an ADAMTS13 activity of 1%, 22%, 57% with platelet counts of 166k, 334k, 224k respectively. These patients had a history of 4, 7 and 8 prior events of TTP, respectively. Following the administration of 4 doses of weekly rituximab 375mg/m2, all had improvement in ADAMTS13 activity to >95%, none requiring TPE. These patients are recurrence-free after 7 months, 19 months, and 3 months of follow-up.
Conclusions: In our single center retrospective study, early use of rituximab does not appear to confer immediate benefit through reduction of TPE or days to platelet normalization. Routine monitoring of ADAMTS13 activity by rapid assay, in conjunction with rituximab therapy as needed, has been shown to effectively normalize ADAMTS13 activity and possibly prevent relapse in three patients with history of relapsed TTP. Our experience provides evidence against the inpatient use of rituximab in relapsed TTP, and provides justification for the development of a protocol for the routine follow-up of TTP patients with implementation of prophylactic rituximab.
Reagan: Teva Pharmaceutical Industries: Membership on an entity's Board of Directors or advisory committees; Alexion Pharmaceuticals: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal