Abstract
Introduction:
Sepsis-associated disseminated intravascular coagulation (SAC) is associated with marked hemostatic changes including transient thrombocytopenia due to their enodogenous activation / consumption. Platelets are decreased in SAC and exhibit compromised function. Patients with SAC are at an increased risk of thrombosis and / or bleeding. The widespread activation of platelets contribute to vascular occlusions, fibrin deposition, multi-organ dysfunction, contributing to a two-fold increase in mortality. At this time there is no single biomarker or laboratory test that can effectively diagnose SAC; however, the International Society on Thrombosis and Hemostasis (ISTH) has introduced a scoring system based on laboratory parameters such as platelet count, clotting time, and levels of markers of thrombosis to calculate SAC severity in terms of DIC score. Measurement of activation markers that describe the interplay between inflammation and platelet function may provide insight into the pathogenesis of SAC. The purpose of this study was to measure markers of platelet function in the plasma of patients with clinically established SAC and to determine their association to disease severity and outcome.
Materials and Methods:
Plasma samples from 103 adult intensive care unit (ICU) patients with sepsis and suspected disseminated intravascular coagulation (DIC) were acquired from the University of Utah Hospital at the time of ICU admission as well as on days 4 and 8. Samples with relevant clinical information were transported to Loyola University Chicago under an IRB-approved protocol and stored at -80˚C prior to analysis. Plasma samples from healthy individuals (n=50) were purchased from George King Biomedical (Overland, KS). DIC scores were calculated using the ISTH scoring algorithm which incorporates platelet count, D-Dimer, INR, and fibrinogen. Patients were categorized as having no DIC, non-overt DIC, or overt DIC. Plasma levels of CD40L, von Willebrand Factor (vWF), platelet factor-4 (PF-4), and microparticles (MP) were quantified using commercially available ELISAs performed according to manufacturer instructions.
Results:
Markers of platelet activation were significantly elevated in patients with sepsis alone and with suspected DIC compared to normal healthy individuals on ICU day 0 (p<0.001). Levels of platelet-associated biomarkers were compared between survivors and non-survivors. PF-4 was significantly decreased in non-survivors compared to survivors (p = 0.0156). No other significant variations based on survival or based on DIC score category were observed.
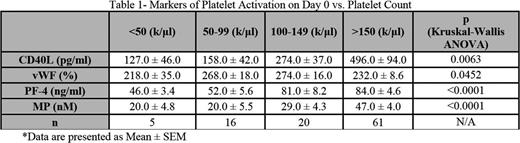
Since platelet count is often dramatically reduced in patients with DIC, the relationship between platelet count and levels of markers of platelet activity was also evaluated. Patients were stratified based on platelet count and levels of markers were compared between groups. CD40L, vWF, PF4, and MP showed significant variation based on platelet count, with all markers exhibiting stepwise elevation with increasing platelet count (Table 1).
Conclusion: Markers of platelet activation were significantly elevated in patients with SAC compared to healthy individuals. This increase was independent of platelet count, underscoring the importance of activation processes to this disease process. Of the markers studied, PF4 showed significant difference based on DIC score or mortality, and differentiated the non-survivors compared to survivors. Levels of CD40L, vWF, PF4, and MP showed significant association with platelet count, increasing in a stepwise manner with increases in platelet count. These studies also suggest that the markers of platelet activation in SAC are primarily regulated by the number of circulating platelets and may be independent of the factors leading to their endogenous consumption.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal