Abstract
Background
Up to 30% of patients (pts) with WM can develop HVS, although serum viscosity (sV) level associated with hyperviscosity-related symptoms in individual pts with WM varies (symptomatic threshold). Also, monoclonal IgMs exhibit a wide range of intrinsic viscosity values with differing individual properties. A recent study proposed that serum IgM level (sIgM) level >6000 mg/dL at diagnosis be considered a new criterion for initiating therapy in otherwise asymptomatic (smoldering) WM to pre-empt the development of HVS.(Gustine et al., BJH 2017) However, the study did not consider patients' sV as information on this parameter was unavailable. We therefore 1) evaluated the predictors of HVS including sV in WM, and 2) assessed the potential value of incorporating the sIgM level at diagnosis into the Consensus criteria for initiating therapy in WM. (Kyle et al., Semin Oncol. 2003)
Methods
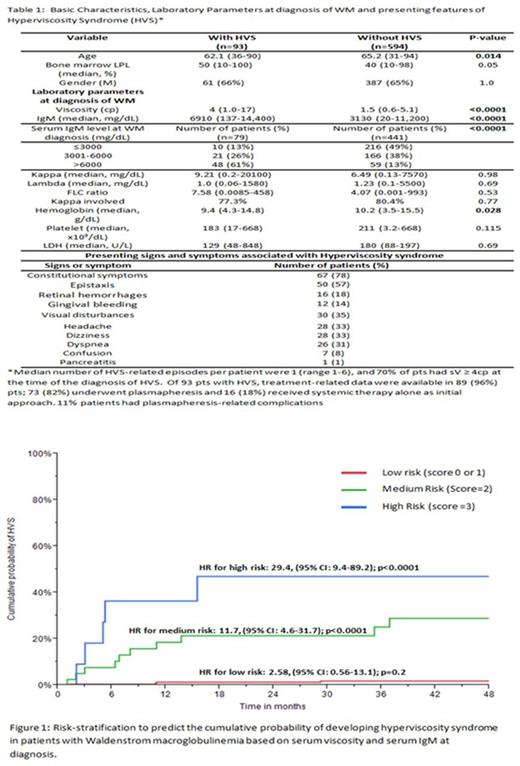
All pts seen at Mayo Clinic, Rochester, between January 1, 01/01/1996 and 06/30/ 2017, in whom a definitive diagnosis of WM was made, were included. HVS was identified by the presence of ≥1 symptoms characteristic of HVS (Stone et al., Blood 2012) that could not otherwise be attributed to another cause. Receiver Operating Characteristic (ROC) curve analysis was used to identify cut-off for continuous variables. Multivariate analysis (MVA) using Cox proportional hazard method was performed to identify independent predictive factors for HVS. Based on this, sV and sIgM at diagnosis of WM were used to formulate a score to predict the cumulative probability of developing HVS in pts who did not present with HVS at diagnosis of WM. sV of 2.2-4.0 cp and sIgM >4,600 mg/dl at diagnosis of WM were given 1 point each and sV >4cp at diagnosis was given 2 points based on hazard ratios (HR) on MVA, allowing for a minimum additive score of 0 and maximum of 3. Kaplan -Meier method was utilized for all time-to-event analyses.
Results
Of 687 pts, HVS was observed in 93 (13.5%) pts, either at the time of diagnosis of WM (n=48) or subsequently during the disease course. The baseline characteristics, presenting symptoms and laboratory parameters of pts with and without HVS, are outlined in Table 1. Optimal cut-offs from ROC curve analysis for sV and sIgM were 2.2 cp and 4600 mg/dL, respectively for predicting the development of HVS. After excluding the pts who developed HVS at diagnosis, a MVA showed that sIgM >4600mg/dL [HR 3.1 (1.3-8.9); p<0.0013] and sV > 2.2 cp [HR 7.6 (3.2-20.5 p<0.0001)] were independent predictors of development of HVS during the subsequent disease course. Scores of 0 and 1 generated similar HRs with overlapping cumulative probability curves for the development of HVS and were therefore categorized as low-risk. After excluding pts with HVS at diagnosis of WM (n=48), the probability of development of HVS during the disease course was highest among pts with sV >4 cp and sIgM >4600 mg/dL (score 3), with 36% cumulative probability of developing HVS at 6 months (Figure 1). Of 520 pts in whom sIgM levels at diagnosis were available, 107 (21%) had a sIgM level >6000 mg/dL. Of these, 83 (78%) pts had one or more indications at diagnosis or instituting systemic therapy per the 2003 Consensus criteria [Hb <10 g/dl, platelets <100 x 109/dL, constitutional symptoms, HVS (n=2)] at diagnosis. Twenty-four pts (22%) with sIgM >6000 mg/dl at diagnosis were otherwise asymptomatic (smoldering WM), not requiring therapy at diagnosis. The median sV for this cohort was 1.6 cp (1.0-4.0 cp) and no pts had sV >4 cp. Of these 24 pts, none developed HVS subsequently, and median time to frontline treatment was 9 years (95% CI 3.6-12.3 years). The median follow-up for the entire cohort was 9.6 years (95% CI: 8.9-10.6) with no difference in the OS in pts with HVS [median OS 9.6 years (95% CI: 6.2-12.3)] versus pts without HVS [median OS 9.7 years (95% CI: 8.8-10.7), p=0.67].
Conclusion
A vast majority of patients with baseline sIgM >6000 mg/dL already have an indication for commencement of therapy based on the 2003 Consensus guidelines. The probability of developing HVS in otherwise asymptomatic patients with sIgM level >6000 mg/dl alone at diagnosis remains low if sV is not taken into account, and high sIgM levels alone at diagnosis may not merit preemptive therapy. A simple scoring system based on sVand sIgM level can reliably predict for the development of HVS in pts who do not present with HVS at diagnosis. Regardless, the overall outcome of pts with WM is unaffected by the development of HVS.
Kumar: Celgene, Millennium/Takeda, Onyx, AbbVie, Janssen, Sanofi, Novartis, Amgen, Genentech, Merck, Oncopeptides, Roche, Skyline Diagnostics: Research Funding; Celgene, Millennium, BMS, Onyx, Janssen, Noxxon, AbbVie, Amgen, Merck, Oncopeptides, Skyline Diagnostics, Takeda: Consultancy; Skyline: Honoraria. Gertz: Celgene, Novartis, Smith-Kline, Prothena, Ionis, Amgen: Honoraria; Millennium: Consultancy, Honoraria. Witzig: Novartis: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Acerta: Research Funding; Kura: Research Funding. Dingli: Karyopharm Therapeutics: Research Funding; Millenium: Consultancy; Takeda: Consultancy; Janssen: Consultancy; Alexion Pharmaceuticals: Consultancy. Dispenzieri: Celgene, Millenium, Pfizer, Janssen: Research Funding. Ansell: Affimed: Research Funding; Bristol-Myers Squibb: Research Funding; Merck: Research Funding; Seattle Genetics: Research Funding; Celldex: Research Funding. Kapoor: Takeda, Celgene and Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal