Abstract
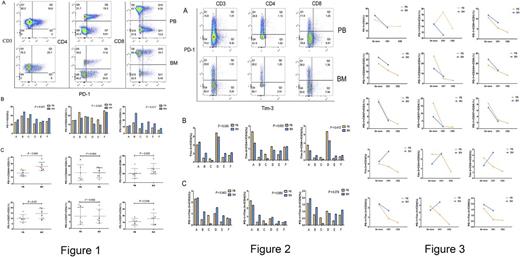
Immunosuppressive microenvironment plays a crucial role for T cell immunodeficiency in multiple myeloma. Increasing data showed that overexpression of the T cell immunosuppressive receptors, such as programmed death-1 (PD-1), cytotoxic T lymphocyte antigen-4 (CTLA-4) and T cell immunoglobulin mucin-3 (Tim-3) may be related to tumor immunosuppression and poor prognosis, and the malignant bone marrow microenvironment may contribute to such immunosupression. In this study, we compared the difference of PD-1 and Tim-3 expression with exhausted CD3+, CD4+ and CD8+ T cells between bone marrow (BM) and peripheral blood (PB) in patients with multiple myeloma (MM). BM and PB samples from 6 cases (4 males and 2 females, age range: 41-82 years old) with untreated MM were selected to this study, the frequencies of PD-1 and Tim-3 expression in CD3+, CD4+ and CD8+ T cells from BM and PB mononuclear cells were detected by Flow cytometry. We also detected the frequency of CD244 and CD57 expression in both CD4+ and CD8+ T cells, which are the immune markers for T cell exhaustion. The change of the frequency of T cell phenotype was followed up in two cases in different time point after therapy. The results showed that significant higher percentage of PD-1+CD3+T cells was found in BM compared with PB (P= 0.001), particularly in PD1+CD8+T cells was significantly higher in BM (P= 0.017), however, interesting, higher percentage of PD-1+CD4+T cells was showed in PB compared with BM (P= 0.043) (Figure 1). Similarly, the percentage of Tim-3+CD3+T cell in BM seemed high compared with PB, as well as in PD-1+Tim-3+CD3+, CD4+ and CD8+T cells. The percentage of CD57+, CD244+ in CD3+, CD4+ and CD8+ T cells was relative high in BM group in comparison with PB group, although the statistical significance was not significant. However, either PD-1+CD244+ (P= 0.006) or PD-1+CD57+( P = 0.02) in CD3+ T cells was significant higher in BM group than that in PB group. Moreover, PD-1+CD244+( P = 0.000) and PD-1+CD57+ (P = 0.048) in CD8+ T cells were higher distributed in BM than that in PB, while there was not significant different in CD4+ T cells (Figure 2). And the limit data also showed that the numbers of either PD-1+ or PD-1+Tim-3+T cells in different T cell subsets were decreases in both BM and PB when the patient achieved complete remission after therapy (Figure 3). In conclusions, we characterized the different distribution of PD-1 and Tim-3 concurrent with exhausted CD3+, CD4+ and CD8+ T cells between BM and PB in patients with MM. Higher numbers of PD-1+CD244+ or PD-1+CD57+ CD3+ T cells in BM from MM patients may contribute to mediate the BM immunosuppressive microenvironment, higher lever PD-1+CD244+ or PD-1+CD57+CD8+T cells may relate to lower T cell activation and T cell immunodeficiency.
Li: Guangdong Provincial Basic Research Program (No. 2015B020227003: Research Funding; National Natural Science Foundation of China (91642111): Research Funding; Guangzhou Science and Technology Project (No. 2015100010211): Research Funding; Guangdong Provincial Applied Science and Technology Research & Development Program (No. 2016B020237006): Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal