Abstract
Introduction
Sepsis is a catastrophic complication of infection which results in systemic inflammatory responses. Inflammasomes initiate the inflammatory cascade that results in the activation of caspase-1 leading to the upregulation of inflammatory cytokines such as IL6 and TNFa. The NRLP-3 inflammasome contributes to the innate immune response identification of pattern recognition receptors (PRRS) on pathogens including bacterial and viruses. While the role of inflammasome in the inflammatory response is known it is not clear how inflammasome contributes to the hemostatic dysregulation observed in sepsis associated coagulopathy. The purpose of this study is to quantitate inflammasome levels in defined sepsis associated patients and to determine its potential relevance to various biomarkers of hemostatic dysregulation.
Materials and Methods:
Plasma samples from 52 adults with sepsis and suspected coagulopathy were analyzed. Samples were collected from patients on ICU day 0 at the University of Utah and were transferred to Loyola under an IRB approved protocol. Samples were stored at -80˚C prior to analysis. Platelet count was determined as part of standard clinical practice. Healthy control samples were purchased from George King Biomedical (Overland, KS). Prothrombin time (PT) / INR was measured using recombiplastin reagent. Fibrinogen was measured using a clot based method on ACL-ELITE coagulation analyzer. Cortisol, D-dimer, PAI-1, NLRP-3 inflammasomes, MP-TF, Fibronectin, and CD40L were measured using commercially available ELISA assays performed according to the manufacturer's instructions.
Results:
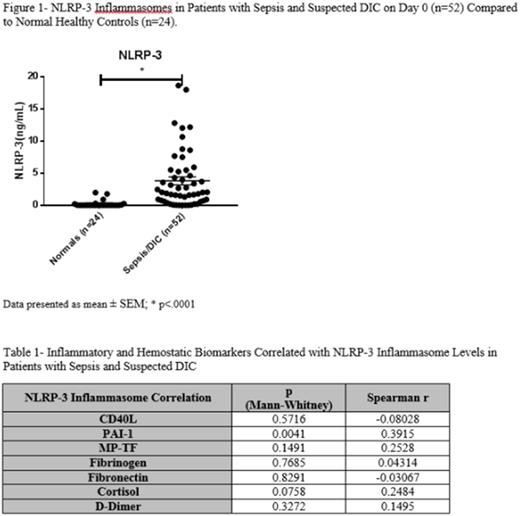
When comparing patients with sepsis and suspected DIC to the normal plasma samples, there was a significant elevation in NLRP-3 inflammasome levels in the sepsis cohort (p = < 0.0001). The NLRP-3 inflammasome concentration in the sepsis cohort did not correlate with other biomarkers. An elevated level of NLRP-3 inflammasomes was significantly associated with an increased levels of PAI-1 (p < 0.0004). No other inflammatory or hemostatic markers were significantly correlated with NLRP-3 inflammasomes.
Conclusion:
The current study shows a significant relationship between inflammasomes and PAI-1 levels in patients with sepsis associated coagulopathy. The positive correlation between NLRP-3 inflammasomes and PAI-1 shows that the activation of inflammasomes may have a role in the upregulation of PAI-1 and the observed hemostatic dysregulation. The strong association between NLRP-3 inflammasome and PAI-1 in baseline samples of patients with sepsis and DIC also suggest that NLRP-3 inflammasome may contribute to the fibrinolytic dysregulation in sepsis and DIC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal