Abstract
Introduction: Cytotoxic chemotherapy is frequently employed in the treatment of aggressive malignancies such as acute myeloid leukemia (AML). Patients (pts) who respond to this therapy universally experience significant cytopenias after a period of bone marrow hypocellularity that is the result of toxicity to normal hematopoietic cells. Older pts with AML poorly tolerate cytotoxic chemotherapy, largely due to these cytopenias, and novel therapies that spare this toxicity are needed. In the setting of a multi-center phase 1b dose escalation/expansion study (NCT02203773), we explored the combination of the BCL-2 inhibitor venetoclax (ven) with azacitidine (aza) for elderly AML pts unfit for induction chemotherapy. We noted distinctive post treatment morphologic appearances of some pts' bone marrow biopsies that could be grouped based on cellularity. This observation, coupled with a high overall response rate that included some pts who did not achieve full count recovery, led to a hypothesis that bone marrow cellularity, either at baseline or after 1 treatment cycle, might predict full vs. incomplete count recovery in the context of this novel therapy.
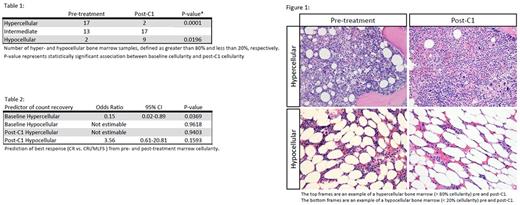
Methods: We enrolled 33 pts at our institution into this dose escalation/expansion study involving the sequential administration of aza at the standard dose and schedule with daily ven; 23 received 400 mg venetoclax, 9 received 800 mg and 1 received 1200 mg. Cycles lasted 28 days and were repeated indefinitely in the absence of progression or limiting toxicity. Baseline and post cycle 1 bone marrow biopsies were assessed as hypercellular (>80% cellularity) or hypocellular (<20% cellularity) (Figure 1). Univariate logistic regression analysis was used to determine whether these features predicted the ability to achieve a complete remission (CR) versus CR with incomplete count recovery (CRi) or morphological leukemia free state (MLFS), and McNemar's test for paired samples was used to predict whether pre-treatment cellularity predicted post-treatment cellularity.
Results: 17 pts at baseline met pre-defined criteria for hypercellularity and 2 were hypocellular. 10/33 pts had AML with myelodysplasia related changes; of these, 6 were hypercellular and none were hypocellular at baseline. After 1 cycle, 2 pts met criteria for hypercellularity and 9 were hypocellular. Hypercellularity at baseline predicted post treatment hypercellularity (P=0.0001) and hypocellularity at baseline predicted post treatment hypocellularity (P=0.0196) (Table 1). Median time to platelet and neutrophil recovery was 25 and 42 days, respectively. Hypercellularity at baseline was significantly associated with a reduced ability to recover blood counts (OR to achieve CR vs. CRi/MLFS was 0.15, 95% CI 0.02-0.89, P=0.0369). Hypocellularity at baseline was not associated with failure to recover blood counts (P=0.9618). Hyper or hypocellularity after cycle 1 did not predict ability to recover counts (p=0.9403 and 0.1593, respectively) (Table 2).
Conclusion: Novel therapies that spare elderly pts long periods of cytopenias are necessary. Ven with aza is an active combination in this population. Although nearly all pts in our cohort achieved an International Working Group defined overall response, several had a CRi or MLFS. After cycle 1 of treatment, some pts achieved a remission without an apparent period of hypocellularity. Surprisingly, hypercellularity at baseline was associated with a lower likelihood of achieving full count recovery after treatment. Patients that were hypercellular after cycle 1 were more likely to have been hypercellular at baseline, however, hypercellularity after cycle 1 was not associated with delayed count recovery. Neither baseline nor post treatment hypocellularity had a higher association with poor count recovery. These observations will need to be tested in a larger sample set, but they suggest that marrow recovery may not be linked to morphologic features like baseline cellularity. In the setting of non-intensive therapies other features may predict inferior count recovery, such as the presence or duration of an antecedent hematologic malignancy like MDS.
Pollyea: Takeda, Ariad, Alexion, Celgene, Pfizer, Pharmacyclics, Gilead, Jazz, Servier, Curis: Membership on an entity's Board of Directors or advisory committees; Agios, Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal