Abstract
Burkitt lymphoma (BL) that is refractory to frontline intensive therapy is generally associated with a dismal outcome. We report a case where this prognosis has apparently been overcome with an intensified variation of the DA EPOCH-R schedule. Wilson and coworkers have developed this infusional schedule with dose modification and it has been reported to achieve excellent outcomes in the first line therapy of BL.
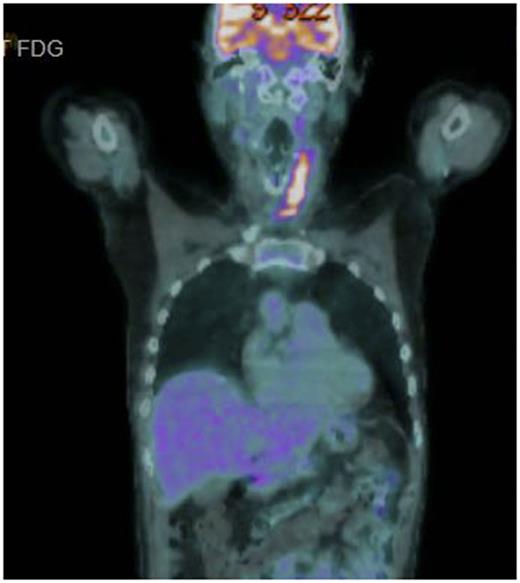
A 56 year old male presented with rapid onset superior vena cava obstruction that caused an intensive care admission at the time of diagnosis. Staging showed stage 2 with neck disease, near complete SVC obstruction and a 6 x 5 x 5cm superior mediastinal mass. Therapy was commenced with R CODOX-M / R IVAC with an initial symptomatic improvement but by the time of recovery from course 2, the symptoms of respiratory distress were recurring in the left neck where partial acute respiratory obstruction occurred. No significant improvement in the neck mass was seen on repeat CT and urgent radiotherapy (R/T) was given to relieve symptoms. Persistent active disease was then confirmed by CT /PET scanning in the left neck (SUV 10.8), an exemplar image of this scan is shown in Figure. The patient was counselled as to the dire prognosis but was unwilling to accept that further intensive treatment was unlikely be successful and requested further chemotherapy. In the light the intensity of the treatment already delivered a novel strategy was conceived and agreed.
Second line treatment was given with the DA EPOCH -R schedule but escalated to dose level 6 from the start of second line therapy. The rationale for this was that the dose intensity needed to be higher than that of the failed front line regimen. Dose limiting mucositis was encountered and the etoposide was reduced to 65% of dose level 6, other drugs remained at dose level 6. By cycle 5, the doxorubicin dose was capped at a total cumulative dose of 450 mg/m2 so as to not exceed a safe cardiac dose. The chemotherapy doses delivered were Etoposide 125 ( 80 from cycle 2) mg/ m2 /day , Vincristine 0.4 mg/ m2/day, Doxorubicin 25 mg/ m2/day (cycle1-4), Cyclophosphamide 1900 mg/ m2 day 5 and rituximab 375 mg/ m2. 5 cycles were delivered in total. The total cumulative hospital inpatient stay during treatment was 58 days.
End of treatment PET showed a complete response which has now been maintained for 12 months. Two attempts at stem cell mobilisation failed, despite the use of plerixifor, so a consolidation autologous stem cell transplant was not pursued. End of treatment radiotherapy to sites of initial disease was implemented after end of treatment restaging.
This is a single case but we believe a good outcome has been achieved in an otherwise near hopeless situation and may provide a useful insight into improving salvage therapy of BL. We believe the strategy of using DA EPOCH R starting at maximum intensity from the start of therapy has not been previously reported. We also acknowledge the courage and stoicism of our patient whose determination to persist with therapy was exceptional. He remains in remission, has an ECOG status of 0 and has returned to work.
McMillan: Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel sponsorship. Bishton: Roche: Other: Travel Sponsorship. Fox: Roche: Consultancy, Honoraria, Other: Travel Sponsorship, Research Funding, Speakers Bureau; AbbVie: Consultancy, Honoraria, Other: Travel Sponsorship, Research Funding; Janssen: Consultancy, Honoraria, Other: Travel Sponsorship, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal