Key Points
Selenoproteins, and in particular SelenoW, are required for stress erythroid progenitor proliferation and maturation.
Macrophages require selenoproteins to maintain erythropoietic niche competency.
Abstract
Micronutrient selenium (Se) plays a key role in redox regulation through its incorporation into selenoproteins as the 21st amino acid selenocysteine (Sec). Because Se deficiency appears to be a cofactor in the anemia associated with chronic inflammatory diseases, we reasoned that selenoproteins may contribute to erythropoietic recovery from anemia, referred to as stress erythropoiesis. Here, we report that loss of selenoproteins through Se deficiency or by mutation of the Sec tRNA (tRNA[Sec]) gene (Trsp) severely impairs stress erythropoiesis at 2 stages. Early stress erythroid progenitors failed to expand and properly differentiate into burst-forming unit-erythroid cells , whereas late-stage erythroid progenitors exhibited a maturation defect that affected the transition of proerythroblasts to basophilic erythroblasts. These defects were, in part, a result of the loss of selenoprotein W (SelenoW), whose expression was reduced at both transcript and protein levels in Se-deficient erythroblasts. Mutation of SelenoW in the bone marrow cells significantly decreased the expansion of stress burst-forming unit-erythroid cell colonies, which recapitulated the phenotypes induced by Se deficiency or mutation of Trsp. Similarly, mutation of SelenoW in murine erythroblast (G1E) cell line led to defects in terminal differentiation. In addition to the erythroid defects, the spleens of Se-deficient mice contained fewer red pulp macrophages and exhibited impaired development of erythroblastic island macrophages, which make up the niche supporting erythroblast development. Taken together, these data reveal a critical role of selenoproteins in the expansion and development of stress erythroid progenitors, as well as the erythroid niche during acute anemia recovery.
Introduction
Steady-state erythropoiesis maintains homeostasis by continuously generating new erythrocytes to replace senescent erythrocytes that are removed by macrophages in the spleen and liver.1 However, when the bone marrow (BM) cannot supply sufficient erythrocytes, stress erythropoiesis predominates. Stress erythropoiesis is best understood in the mouse, where it is extramedullary, occurring in the fetal liver and adult spleen and liver. Unlike steady-state erythropoiesis, which constantly generates erythrocytes, stress erythropoiesis generates a wave of new erythrocytes designed to maintain homeostasis until the BM can resume erythroid production.2,3 Stress erythroid progenitors (SEPs) are distinct from steady-state progenitors in that they are derived directly from short-term reconstituting hematopoietic stem cells, which become erythroid restricted on migration to the spleen.4 Furthermore, stress erythropoiesis uses signals, including bone morphogenetic protein 4 (Bmp4), Hedgehog (Hh), and growth and differentiation factor 15 (Gdf15), that do not regulate steady-state erythropoiesis.5-9 These signals, along with stem cell factor, promote the rapid expansion of a self-renewing stem cell-like population of early SEPs, which are unable to differentiate until the rise in serum erythropoietin (Epo) levels promotes their transition to stress burst-forming unit-erythroid cells (BFU-Es).4,6,10 Although stress erythropoiesis uses specialized progenitors, terminal differentiation requires similar Epo-dependent signaling events, as required in steady-state erythropoiesis. For these events, GATA-1 serves as the central transcription factor that promotes the erythroid differentiation program, which culminates in the expression of globin proteins and heme synthesis to form hemoglobin.11-14 Throughout this process, proliferation and differentiation of progenitors are highly coordinated so that sufficient new erythrocytes are produced to counteract anemic stress.5-9
Erythroid cells develop within specialized niches referred to as erythroblastic islands (EBIs), which involves interaction between the erythroid cells and macrophages.15 In vivo depletion of macrophages compromises stress erythropoiesis.16-18 The crosstalk in the niche relies on direct macrophage–erythroblast interactions mediated by adhesion molecules.15,19,20 Macrophages provide survival and proliferation signals to erythroblasts and promote erythroblast enucleation.15,16,21 In addition, macrophages play an important role in heme-iron recycling and heme-dependent signaling in the spleen.22-25 Bach1 is a transcriptional repressor that is degraded when bound to heme.26 This regulation affects both erythroid development and macrophage development. Bach1 inhibits α and β globin expression, limiting hemoglobin production.26,27 Similarly, it inhibits the expression of SpiC, a transcription factor required for the development of red pulp macrophages (RPMs).28-30 Therefore, disruption of heme homeostasis causes excess oxidative stress, leading to cell injury and impaired erythropoiesis.31,32
Selenium (Se) in selenoproteins occurs as the 21st amino acid, selenocysteine (Sec). In response to exogenous Se supply, Sec is incorporated via a highly orchestrated process involving the tRNA[Sec] (encoded by Trsp) that decodes the UGA codon, which is critical for the redox activity of selenoproteins.33 Se and selenoproteins exert a wide range of effects in human health. Apart from cardiomyopathy as seen in Keshan disease, Se deficiency appears to be a cofactor in the anemia associated with chronic inflammatory diseases.34-36 Furthermore, previous studies indicate a protective role for Se and selenoproteins in erythrocytes from oxidative damage.37-40 However, the physiological functions of specific selenoproteins that are involved in erythropoiesis remain unclear.
In this study, we demonstrate that loss of selenoproteins through diet-induced deficiency or genetic deletion of the selenoproteome severely compromises stress erythropoiesis, negatively affecting expansion of early SEPs and maturation of erythroblasts. Our data also suggest that selenoprotein W (SelenoW) plays a role in regulating the proliferation of stress BFU-Es and the transition from proerythroblasts (ProEs) to basophilic erythroblasts (BasoEs). Furthermore, the loss of selenoproteins leads to defects in EBIs. These data show that selenoproteins are required for efficient stress erythropoiesis at multiple levels.
Methods
Detailed study design and methods are described in supplemental Methods, available on the Blood Web site.
Mice
Three-week-old C57BL/6 mice were maintained either on a Se-deficient (<0.01 ppm Se; Se-D) or Se-adequate (0.08 ppm Se; Se-A) diet (Harlan) for 12 weeks. C57BL/6-Trspfl/flLysMCre mice were a gift from Dolph Hatfield (National Cancer Institute, National Institutes of Health). C57BL/6-Trspfl/Δ strain was generated by crossing C57BL/6-Trspfl/fl with B6.C-Tg (CMV-Cre) lCgn/J mice (JAX: 006054). C57BL/6-Trspfl/Δ; GT (Rosa)26SORTM1(CreERT2)Tyj/J strain (Trspfl/Δ;CreERT) was generated by crossing C57BL/6-Trspfl/Δ mice with B6.129-GT(Rosa)26SORTM1(CreERT2)Tyj/J (JAX: 008463). Cas9-dependent gene editing was performed using C57BL/6-Gt(Rosa)26Sortm1.1(CAG-Cas9-EGFP)Fezh/J (TgCas9-GFP, JAX: 026179)41 All procedures were approved by the Institutional Animal Care and Use Committee of Pennsylvania State University.
Phenylhydrazine treatment
Mice were injected intraperitoneally with phenylhydrazine (PHZ) at a dose of 100 mg/kg or 50 mg/kg body weight. Peripheral blood was collected for hematocrit measurement. Serum Epo (MEP00B; R&D) and corticosterone levels (ADI-901-097; Enzo) were measured by ELISA.
Bone marrow transplantation
In the short-term radioprotection model, Trspfl/fl recipient mice were lethally irradiated (950 Gy) and were transplanted with 0.5 × 106 whole bone marrow (BM) cells by retro-orbital injection. TrspΔ/Δ and control Trspfl/Δ donor cells were generated by treatment with 4-hydroxytamoxifen in vitro for 48 hours before transplant. To generate a hematopoietic-specific knockout of Trsp, Trspfl/fl recipient mice were transplanted with 0.5 × 106Trspfl/Δ;CreERT or Trspfl/Δ BM donor cells. Mice were allowed to engraft for 8 weeks, followed by intraperitoneal injection of tamoxifen (Sigma) in corn oil at 75 mg/kg body weight.
Statistical analysis
All quantitative data were represented as mean ± SEM of at least duplicate biological replicates. A Student t test was used for analyses of difference between 2 groups. ANOVA was used for analyzing data with more than 2 groups with Holm-Sidak test adjustment for multiple comparisons. Significance level was set at α = 0.05.
Results
Se deficiency impairs stress erythropoiesis
Previously we reported Se-D mice exhibited anemia despite an increase in spleen BFU-Es,37 suggesting that stress erythropoiesis in Se-D mice may be impaired. We used a PHZ-induced (10 mg/kg, 100% PHZ) acute hemolytic anemia mouse model to test this idea further (Figure 1A). Although the control Se-A mice were able to recover from anemia in approximately 7 days, none of the Se-D mice survived beyond 3 days, and they failed to generate new reticulocytes or erythrocytes, leading to lethal anemia with severe hemolysis (Figure 1B-D; supplemental Figure 1A). Analysis of the spleen weight and histopathology suggested defective expansion of SEPs with significantly decreased histopathological evidence of stress erythropoiesis in the Se-D mice (Figure 1E-F). Examination of splenic stress BFU-Es indicated a twofold increase in the Se-A mice between days 2 and 3 posttreatment, but no increase was observed in the Se-D group (Figure 1G, left). Furthermore, colony sizes were relatively smaller in the Se-D mice (Figure 1G, right). These data clearly indicated defective expansion of erythroid cells in the Se-D mice. However, this difference was not caused by defective expression of key growth factors required for stress erythropoiesis (supplemental Figure 1B-E).
Se deficiency impairs stress erythropoiesis after PHZ administration. (A) Schematic of the study model. C57BL/6 mice were fed on a Se-D or Se-A diet for 12 weeks before use. Then mice were treated with PHZ (100 mg/kg [100%] or 50 mg/kg [50%]). Kinetics of stress erythropoiesis were evaluated by time course study. (B-G) Kinetics of stress erythropoietic recovery of Se-D and Se-A mice treated with 100% PHZ. (B) Survival curve of mice over the course of 12 days of recovery; n = 8 per diet. (C) Hematocrit measurements of mice during the recovery from PHZ-induced anemia; n = 10-15 per diet. (D) Normalized reticulocyte percentage in the whole blood at days 1.5 and 2.5 after PHZ treatment; n = 3 per diet. (E) Spleen weights (left) and the representative pictures of spleens (right) from mice on the different diets on the indicated days after PHZ treatment; n = 3-7 per diet. (F) Hematoxylin and eosin staining of spleen sections from Se-D and Se-A mice on the indicated days after PHZ treatment (original magnification ×100). (G) Stress BFU-E colony assays of spleen cells isolated from Se-D and Se-A mice at indicated times after PHZ treatment (left) and representative pictures of BFU-E colony morphology on day 3 posttreatment (right; acid benzidine stain; original magnification ×50); n = 3-6 per diet. Bars are representative of mean ± SEM. **P < .001; ***P < .005; ****P < .0001.
Se deficiency impairs stress erythropoiesis after PHZ administration. (A) Schematic of the study model. C57BL/6 mice were fed on a Se-D or Se-A diet for 12 weeks before use. Then mice were treated with PHZ (100 mg/kg [100%] or 50 mg/kg [50%]). Kinetics of stress erythropoiesis were evaluated by time course study. (B-G) Kinetics of stress erythropoietic recovery of Se-D and Se-A mice treated with 100% PHZ. (B) Survival curve of mice over the course of 12 days of recovery; n = 8 per diet. (C) Hematocrit measurements of mice during the recovery from PHZ-induced anemia; n = 10-15 per diet. (D) Normalized reticulocyte percentage in the whole blood at days 1.5 and 2.5 after PHZ treatment; n = 3 per diet. (E) Spleen weights (left) and the representative pictures of spleens (right) from mice on the different diets on the indicated days after PHZ treatment; n = 3-7 per diet. (F) Hematoxylin and eosin staining of spleen sections from Se-D and Se-A mice on the indicated days after PHZ treatment (original magnification ×100). (G) Stress BFU-E colony assays of spleen cells isolated from Se-D and Se-A mice at indicated times after PHZ treatment (left) and representative pictures of BFU-E colony morphology on day 3 posttreatment (right; acid benzidine stain; original magnification ×50); n = 3-6 per diet. Bars are representative of mean ± SEM. **P < .001; ***P < .005; ****P < .0001.
Se-D mice attempted to compensate for these defects in stress erythropoiesis by increasing levels of serum corticosteroid and Epo approximately two- to threefold (supplemental Figure 1F-G). Despite the increase in serum Epo, the levels of kidney Epo mRNA were comparable (supplemental Figure 1H). Characterization of peripheral blood mononuclear cells showed that there were proportionally more CD34+CD133+Kit+Sca1+ erythroid progenitors10 migrating in the periphery of the Se-D mice compared with the Se-A mice (supplemental Figure 1I-J). They generated two- and sixfold more stress BFU-Es on day 1.5 and day 2.5 after PHZ treatment, respectively (supplemental Figure 1K). Our previous data showed that short-term reconstituting hematopoietic stem cells migrate from the BM to the spleen to replenish SEPs in the spleen.4 This increase in SEPs in the peripheral blood suggests that Se-D mice are attempting to compensate for their inability to respond to the anemia.
Expansion of SEPs requires Se
As none of the Se-D mice survived 100% PHZ treatment, to further characterize their defects, a reduced dose of PHZ (50 mg/kg, 50% PHZ; Figure 1A) was used, where 10% of Se-D mice survived and recovered from the treatment (Figure 2A-B). We observed more cell death in Se-D mice because of necrosis, as opposed to apoptosis in Se-A mice (supplemental Figure 2A-B). In addition, there was increased reactive oxygen species production in spleen cells of the Se-D mice (supplemental Figure 2C), indicating high oxidative stress. Se deficiency also significantly affected the differentiation of early Kit+CD133+ SEPs to more mature Kit+CD133− SEPs (Figure 2C-D).
Se and selenoproteins are required in early SEPs. (A-D) Analysis of Se-A and Se-D mice treated with 50% PHZ. (A) Survival of Se-A and Se-D mice treated with 50% PHZ; n = 8 per diet. (B) Analysis of hematocrit during recovery from treatment with 50% PHZ; n = 10-15 per diet. (C) Representative flow cytometry graphs of Kit+CD133+early SEPs during recovery from PHZ treatment. (D) Quantitation of spleen Kit+CD133+early SEPs and Kit single-positive cells during recovery; n = 3-4 per diet. (E-F) In vitro analysis of TrspΔ/Δ and control cells using 2-phase stress erythropoiesis culture; n = 4 per group. (E) Total cell numbers postexpansion culture (in stress erythropoiesis expansion medium [SEEM]) and differentiation culture (in stress erythropoiesis differentiation medium [SEDM]). (F) Stress BFU-E colony assays of cells after differentiation culture. (G-J) In vivo short-term radioprotective model. Donor BM cells were obtained from Trspfl/Δ;CreERT or control Trspfl/Δ mice. Trsp gene deletion was induced by treating cells with 4-hydroxytamoxifen in vitro 48 hours before bone marrow transplant. (G) Survival rate and (H) hematocrit measurements of transplanted mice on the indicated days posttransplant. Two independent repeats; n = 5 for each group. (I) Total spleen SEPs on days 8 and 10 after BMT; n = 4 per group. (J) Stress BFU-E colony assays of spleen cells on day 10 after BMT; n = 4 per group. Bars are representative of mean ± SEM. *P < .05; ***P < .005; ****P < .0001.
Se and selenoproteins are required in early SEPs. (A-D) Analysis of Se-A and Se-D mice treated with 50% PHZ. (A) Survival of Se-A and Se-D mice treated with 50% PHZ; n = 8 per diet. (B) Analysis of hematocrit during recovery from treatment with 50% PHZ; n = 10-15 per diet. (C) Representative flow cytometry graphs of Kit+CD133+early SEPs during recovery from PHZ treatment. (D) Quantitation of spleen Kit+CD133+early SEPs and Kit single-positive cells during recovery; n = 3-4 per diet. (E-F) In vitro analysis of TrspΔ/Δ and control cells using 2-phase stress erythropoiesis culture; n = 4 per group. (E) Total cell numbers postexpansion culture (in stress erythropoiesis expansion medium [SEEM]) and differentiation culture (in stress erythropoiesis differentiation medium [SEDM]). (F) Stress BFU-E colony assays of cells after differentiation culture. (G-J) In vivo short-term radioprotective model. Donor BM cells were obtained from Trspfl/Δ;CreERT or control Trspfl/Δ mice. Trsp gene deletion was induced by treating cells with 4-hydroxytamoxifen in vitro 48 hours before bone marrow transplant. (G) Survival rate and (H) hematocrit measurements of transplanted mice on the indicated days posttransplant. Two independent repeats; n = 5 for each group. (I) Total spleen SEPs on days 8 and 10 after BMT; n = 4 per group. (J) Stress BFU-E colony assays of spleen cells on day 10 after BMT; n = 4 per group. Bars are representative of mean ± SEM. *P < .05; ***P < .005; ****P < .0001.
Loss of selenoproteins through mutation of Trsp blocks the expansion of SEPs
To further elucidate the role of selenoproteins in stress erythropoiesis, we used mice with a conditional allele of Trsp (Trspfl/Δ;CreERT). Although Se deficiency significantly decreases selenoprotein expression, Trsp deletion causes complete knockout of selenoproteins.33 BM cells from Trspfl/Δ;CreERT and control Trspfl/Δ mice were plated in the stress erythropoiesis 2-stage culture system10 after Trsp deletion (supplemental Figure 2D). Significantly fewer mutant cells expanded during the expansion stage, and only a few mutant cells grew in the differentiation culture without any stress BFU-E formation (Figure 2E-F; supplemental Figure 2F). In addition, TrspΔ/Δ BM cells were defective in forming granulocyte-macrophage colonies, indicating a multilineage defect affecting multipotent progenitors (supplemental Figure 2E-F). To translate these results in vivo, bone marrow transplantation (BMT) was performed where SEPs provide erythroid short-term radioprotection.4 The recipients of TrspΔ/Δ BM cells failed to survive past day 10 post-BMT and died of lethal anemia (Figure 2G-H). The spleen sizes were significantly smaller and total cell numbers were less in the mutant group on days 8 and 10 after BMT (supplemental Figure 2G-H). Notably, there were significantly reduced SEPs in spleens of mice in the mutant group that failed to form stress BFU-E colonies (Figure 2I-J). We expanded this analysis in chimeric mice by transplanting Trspfl/Δ;CreERT and control donor BM cells into wild-type recipient mice. Eight weeks after transplant, the mice were treated with tamoxifen and challenged with PHZ treatment (supplemental Figure 2I). This conditional knockout of Trsp in the hematopoietic compartment of mice resulted in fewer SEPs in the spleens on day 2 after PHZ treatment, and a delayed of hematocrit recovery compared with the control mice (supplemental Figure 2J-K). This result confirmed that the defects occurred directly in erythroid lineage. The milder phenotypes were not surprising given that SEPs generated before Trsp deletion, which were still capable of responding to stress. Taken together, these data strongly support the key role for Se and selenoproteins in the expansion and differentiation of SEPs in stress conditions induced by PHZ and irradiation.
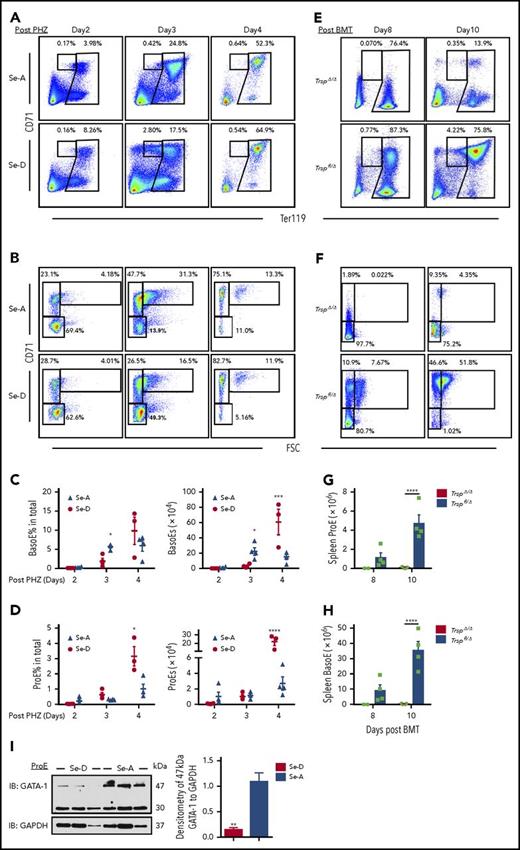
Selenoprotein deficiency impairs terminal maturation of erythroblasts
BFU-Es generate erythroblasts that mature into erythrocytes through a series of intermediate precursors characterized by differential expression of CD71 and Ter119.42,43 Delayed terminal maturation was observed in Se-D mice. There were significantly fewer splenic BasoEs, but similar numbers of ProEs in Se-D mice compared with Se-A mice on day 3 after 50% PHZ treatment (Figure 3A-D), indicating a delayed transition from ProEs to BasoEs in Se-D mice. Further characterization of Ter119hiCD71loFSClo terminal cells with CD44 revealed that there was a lack of mature erythrocyte formation in the Se-D mice, which were otherwise present in the Se-A mice on day 2 after PHZ treatment (supplemental Figure 3A). Upon reexamining the 100% PHZ-treated mice, we observed delayed BasoEs formation with an accumulation of ProEs in Se-D mice on days 1.5 and 2.5 (supplemental Figure 3B-E). Furthermore, the level of reactive oxygen species in BasoEs was remarkably higher in Se-D mice than Se-A mice on day 3 after 50% PHZ treatment, but comparable in ProEs (supplemental Figure 3F-G). Complete loss of selenoproteins in SEPs leads to a more severe defect. Control (Trspfl/Δ) transplanted mice exhibited CD71loTer119+ cells that were released into circulation by day 10. There was an increase in CD71hiTer119+ cells between days 8 and 10, with this population becoming the predominate population at day 10. These cells represented the synchronous maturation of stress BFU-Es. Similar to the controls, mice transplanted with TrspΔ/Δ BM cells showed a decrease in CD71loTer119+ cells from days 8 to 10. In contrast, there were few CD71hiTer119+ erythroblasts observed on day 8 or 10 of mice transplanted with TrspΔ/Δ BM cells (Figure 3E-H).These data are consistent with the in vitro culture of TrspΔ/Δ BM cells, which failed to expand early progenitor cells and generate stress BFU-Es (Figure 2E-F). Together, these data suggest that loss of selenoproteins severely compromises the development of SEPs before erythroblast maturation, leading to complete loss of erythroblasts in the spleen.
Se deficiency impairs erythroblast maturation. (A-B) Flow cytometry analysis and representative graphs of splenic erythroblasts after 50% PHZ treatment. (A) ProEs and (B) BasoEs are characterized by CD71hiTer119int and CD71hiTer119hiFSChi, respectively. (C) Percentage BasoEs (left) and total numbers of BasoEs (right) isolated from the spleens of Se-A and Se-D mice on the indicated days after 50% PHZ treatment; n = 4 per diet. (D) Percentage ProEs (left) and total numbers of ProEs (right) isolated from the spleens of Se-A and Se-D mice on the indicated days after 50% PHZ treatment; n = 4 per diet. (E-H) Characterization of erythroblasts from TrspΔ/Δ or control cells transplanted mice on days 8 and 10 after BMT. (E) Flow cytometry analysis of total erythroblasts and (F) Ter119hi cells. (G) Quantitation of spleen ProEs and (H) BasoEs. (I) Western blot analysis (left) and densitometry (right) of GATA-1 in sorted splenic ProEs from mice on day 3 after 50% PHZ treatment; n = 3 per diet. Bars are representative of mean ± SEM. Panels B and F were gated on Ter119hi cells. *P < .05; **P < .001; ***P < .005; ****P < .0001.
Se deficiency impairs erythroblast maturation. (A-B) Flow cytometry analysis and representative graphs of splenic erythroblasts after 50% PHZ treatment. (A) ProEs and (B) BasoEs are characterized by CD71hiTer119int and CD71hiTer119hiFSChi, respectively. (C) Percentage BasoEs (left) and total numbers of BasoEs (right) isolated from the spleens of Se-A and Se-D mice on the indicated days after 50% PHZ treatment; n = 4 per diet. (D) Percentage ProEs (left) and total numbers of ProEs (right) isolated from the spleens of Se-A and Se-D mice on the indicated days after 50% PHZ treatment; n = 4 per diet. (E-H) Characterization of erythroblasts from TrspΔ/Δ or control cells transplanted mice on days 8 and 10 after BMT. (E) Flow cytometry analysis of total erythroblasts and (F) Ter119hi cells. (G) Quantitation of spleen ProEs and (H) BasoEs. (I) Western blot analysis (left) and densitometry (right) of GATA-1 in sorted splenic ProEs from mice on day 3 after 50% PHZ treatment; n = 3 per diet. Bars are representative of mean ± SEM. Panels B and F were gated on Ter119hi cells. *P < .05; **P < .001; ***P < .005; ****P < .0001.
Activation of death receptors similar to the tumor necrosis factor receptor results in caspase-3-mediated cleavage of GATA-1 that inhibits the transition of ProEs to BasoEs44,45 (supplemental Figure 3I). We observed cleaved GATA-1 product and significantly reduced levels of the full-length GATA-1 protein in splenic ProEs from Se-D compared with Se-A mice on day 3 after 50% PHZ treatment (Figure 3I), yet irrelevant to apoptosis (supplemental Figure 3H). There were no differences in GATA-1 mRNA levels (data not shown). In addition, the ProE to BasoE transition was also associated with increased cleavage of Lamin B (supplemental Figure 3I), which promotes opening of the nuclear pore to expel histones as an initial step in enucleation.46 Consistent with this paradigm, we observed decreased levels of cleaved Lamin B in Se-D ProEs compared with Se-A ProEs (supplemental Figure 3J). Together, these data underscore the defects that delay the transition from ProEs to BasoEs under Se-D conditions.
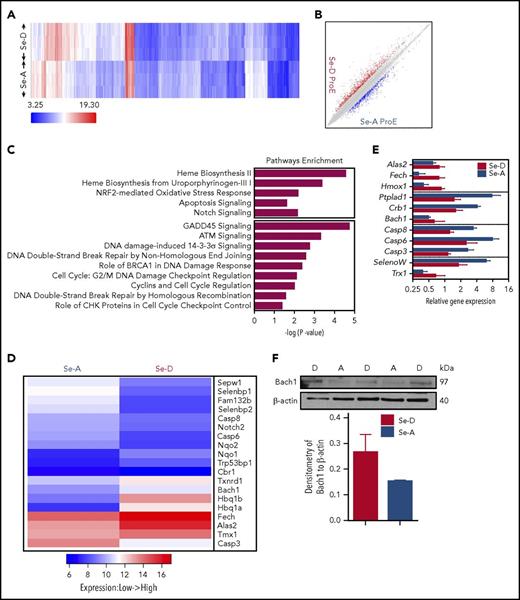
Decreased SelenoW expression in Se-D mice contributes to the defects in terminal erythroid maturation
To better understand how selenoproteins regulate stress erythropoiesis, we performed transcriptomic analysis on splenic ProEs and BasoEs from the Se-D and Se-A mice on day 3 after 50% PHZ treatment, which revealed significant differences in gene expression between the 2 groups (Figure 4A-B; supplemental Figure 4A-B). Ingenuity pathway analysis revealed enriched pathways, including heme synthesis, oxidative stress control, cell death, cell cycle control, erythroid cell growth, and proliferative signaling pathways (Figure 4C; supplemental Figure 4C). Differential expression of key genes from these pathways was confirmed by quantitative polymerase chain reaction (Figure 4D-E). Notably, the heme synthesis pathway in the Se-D ProEs was activated, represented by upregulation of 5′-aminolevulinate synthase 2 (Alas2) and ferrochelatase (Fech), indicating increased cellular heme demand. Low intracellular heme levels also supported by western immunoblotting analysis showed increased expression of Bach1 protein in the Se-D ProEs (Figure 4F). Consistently, the Nrf2 pathway was suppressed, as suggested by decreased expression of 3-hydroxyacyl-CoA dehydratase 3 (Ptplad1) and Crumbs homolog 1 (Crb1) in the Se-D ProEs. This insufficiency in heme biosynthesis is consistent with our previous work showing increased Heinz bodies and precipitation of globins associated with erythrocyte membranes in the Se-D mice.37
Transcriptomic analysis of ProEs during stress erythropoiesis. (A-B) Affymetrix transcriptomic analysis of sorted splenic ProEs from Se-D or Se-A mice on day 3 after 50% PHZ treatment; n = 3 per diet. (A) Heat map of gene hierarchical clustering analysis with cutoff at |fold change|> 2. (B) Scatter plot of gene differential expression analysis with cutoff at |fold change|> 2. (C) Pathway enrichment analysis. Pathways of interest with P < .05 are shown. (D) Heat map representation of specific gene expression differences. (E) Quantitative reverse transcription polymerase chain reaction analysis of specific genes to confirm differential expression. RNA was isolated from ProEs sorted from Se-D and Se-A mice on day 3 after 50% PHZ treatment. (F) Western blot analysis (top) and densitometry (bottom) of Bach1 in sorted splenic ProEs from mice on day 3 after 50% PHZ treatment; n = 2-3 per diet. Bars are representative of mean ± SEM.
Transcriptomic analysis of ProEs during stress erythropoiesis. (A-B) Affymetrix transcriptomic analysis of sorted splenic ProEs from Se-D or Se-A mice on day 3 after 50% PHZ treatment; n = 3 per diet. (A) Heat map of gene hierarchical clustering analysis with cutoff at |fold change|> 2. (B) Scatter plot of gene differential expression analysis with cutoff at |fold change|> 2. (C) Pathway enrichment analysis. Pathways of interest with P < .05 are shown. (D) Heat map representation of specific gene expression differences. (E) Quantitative reverse transcription polymerase chain reaction analysis of specific genes to confirm differential expression. RNA was isolated from ProEs sorted from Se-D and Se-A mice on day 3 after 50% PHZ treatment. (F) Western blot analysis (top) and densitometry (bottom) of Bach1 in sorted splenic ProEs from mice on day 3 after 50% PHZ treatment; n = 2-3 per diet. Bars are representative of mean ± SEM.
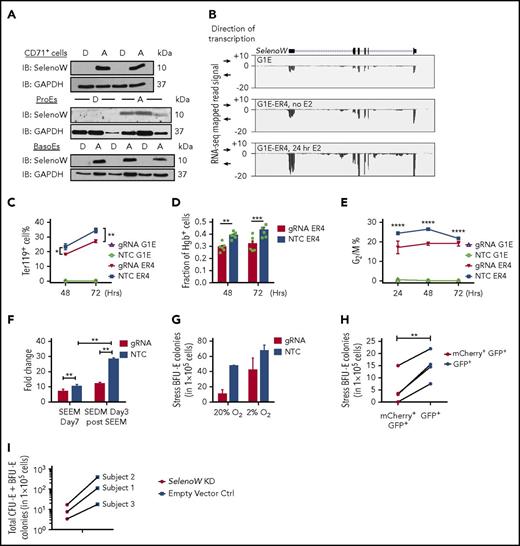
Among the selenoproteins, thioredoxin reductase 1 (Txnrd1), a housekeeping oxidoreductase, was upregulated in Se-D ProEs (Figure 4D-E), in response to increased oxidative stress (supplemental Figure 2C). SelenoW was the only selenoprotein whose gene expression decreased in Se-D ProEs (Figure 4D-E), but not in BasoEs (supplemental Figure 4D), suggesting its participation in the erythroid differentiation. We further confirmed SelenoW protein expression in primary splenic ProEs, BasoEs, and CD71+ cells from PHZ-treated mice, which was absent in all Se-D cells (Figure 5A). Deletion of Trsp gene also led to a loss of SelenoW protein (supplemental Figure 5A). To understand the functions of SelenoW, we used a murine proerythroblast cell line, G1E cells, and its variant G1E-ER4 cells that express a β-estradiol (E2)-inducible GATA-1 protein.47 RNA-Seq data (from ENCODE Project) showed that SelenoW expression was highly upregulated after GATA-1 induction in G1E-ER4 cells compared with the GATA-1 null G1E cells (Figure 5B). Furthermore, chromatin immunoprecipitation-seq data clearly showed GATA-1 binding at SelenoW gene locus (supplemental Figure 5C), suggesting SelenoW as a plausible target of GATA-1. After SelenoW deletion (supplemental Figure 5D), induction of GATA-1 with E2 in SelenoW knockout cells (KO-ER4) resulted in fewer Ter119+ cells and fewer hemoglobin-positive cells, as measured by neutral benzidine staining (Figure 5C-D; supplemental Figure 5E). However, total cellular heme levels were similar in KO-ER4 and control cells (supplemental Figure 5F), suggesting SelenoW affected differentiation, but not the hemes level, during erythroblast maturation. Previously, SelenoW has been implicated in cell cycle regulation.48-50 Cell cycle-related pathways were also enriched in our microarray data set (Figure 4C). Furthermore, lack of SelenoW prevented the decrease in S-phase G1E-ER4 cells, and there were fewer cells in G2/M phase, with no apparent differences in G0/G1phase (Figure 5E; supplemental Figure 5G). Taken together, these data show that mutation of SelenoW causes abnormal terminal differentiation in erythroblasts.
SelenoW is a candidate regulator of erythroid maturation. (A) Protein expression analysis by western blot of SelenoW in sorted spleen CD71+cells, ProEs and BasoEs from Se-D and Se-A mice on day 3 after 50% PHZ treated; n = 2-3. (B) ENCODE RNA-Seq analysis of SelenoW in G1E and G1E-ER4 cells after GATA-1 activation by E2 treatment. (C-E) Analysis of SelenoW knockdown or control G1E and G1E-ER4 cells after E2 treatment. (C) Percentage of Ter119+ cells (n = 3) and (D) percentage of neutral benzidine+ cells (n = 6) generated 48 and 72 hours after treatment with E2 in G1E and G1E-ER4 cells transduced with SelenoW gRNA or a nontargeting control gRNA. (E) Analysis of cell cycle in SelenoW mutant or control G1E-ER4 cells. Percentage of G2/M phase cells in the culture; n = 3. (F-H) SelenoW knockdown in TgCas9-GFP BM cells. SelenoW gRNA was expressed from mCherry-expressing lentivirus. GFP+mCherry+ cells are transduced cells. GFP single-positive (GFP+) cells are nontransduced cells. (F) Fold increase in the percentage of GFP+mCherry+ cells transduced with SelenoW gRNA (gRNA) or nontargeting control gRNA (NTC) after 7 days in SEEM expansion culture and after switching the cultures to 3-day differentiation culture (SEDM day 3 after SEEM). Two independent repeats. (G) Analysis of stress BFU-E colonies generated in the 2-phase culture. Cells were plated after 3 days in SEDM media. Cell were plated in methylcellulose media containing only Epo at 20% O2 or supplemented with BMP4 and stem cell factor at 2% O2. Two independent repeats. (H) Stress BFU-E colony assays of sorted GFP+mCherry+ or GFP+ cells from SelenoW gRNA transduced cultures after 2-phase culture. Cells were plated in methylcellulose media containing only Epo at 20% O2; n = 4 per type of cells. Pairwise Student t test was used for statistical analysis. (I) Colony assays of human BM cells after 2-stage stress erythroid culture. Frozen human bone marrow cells from 3 subjects were thawed 24 hours before transduction with huSelenoW dCas9-KRAB/sgRNA lentivector or dCas9-KRAB empty lentivector control. The cells were transduced by spinoculation, and left in culture with virus overnight. On the second day, cells were transferred to SEEM and cultured for 7 days, followed by 3-day SEDM culture. Transduced (GFP+) cells were purified by sorting and plated for colonies. Bars are representative of mean ± SEM. *P < .05; **P < .001; **P < .005; ****P < .0001.
SelenoW is a candidate regulator of erythroid maturation. (A) Protein expression analysis by western blot of SelenoW in sorted spleen CD71+cells, ProEs and BasoEs from Se-D and Se-A mice on day 3 after 50% PHZ treated; n = 2-3. (B) ENCODE RNA-Seq analysis of SelenoW in G1E and G1E-ER4 cells after GATA-1 activation by E2 treatment. (C-E) Analysis of SelenoW knockdown or control G1E and G1E-ER4 cells after E2 treatment. (C) Percentage of Ter119+ cells (n = 3) and (D) percentage of neutral benzidine+ cells (n = 6) generated 48 and 72 hours after treatment with E2 in G1E and G1E-ER4 cells transduced with SelenoW gRNA or a nontargeting control gRNA. (E) Analysis of cell cycle in SelenoW mutant or control G1E-ER4 cells. Percentage of G2/M phase cells in the culture; n = 3. (F-H) SelenoW knockdown in TgCas9-GFP BM cells. SelenoW gRNA was expressed from mCherry-expressing lentivirus. GFP+mCherry+ cells are transduced cells. GFP single-positive (GFP+) cells are nontransduced cells. (F) Fold increase in the percentage of GFP+mCherry+ cells transduced with SelenoW gRNA (gRNA) or nontargeting control gRNA (NTC) after 7 days in SEEM expansion culture and after switching the cultures to 3-day differentiation culture (SEDM day 3 after SEEM). Two independent repeats. (G) Analysis of stress BFU-E colonies generated in the 2-phase culture. Cells were plated after 3 days in SEDM media. Cell were plated in methylcellulose media containing only Epo at 20% O2 or supplemented with BMP4 and stem cell factor at 2% O2. Two independent repeats. (H) Stress BFU-E colony assays of sorted GFP+mCherry+ or GFP+ cells from SelenoW gRNA transduced cultures after 2-phase culture. Cells were plated in methylcellulose media containing only Epo at 20% O2; n = 4 per type of cells. Pairwise Student t test was used for statistical analysis. (I) Colony assays of human BM cells after 2-stage stress erythroid culture. Frozen human bone marrow cells from 3 subjects were thawed 24 hours before transduction with huSelenoW dCas9-KRAB/sgRNA lentivector or dCas9-KRAB empty lentivector control. The cells were transduced by spinoculation, and left in culture with virus overnight. On the second day, cells were transferred to SEEM and cultured for 7 days, followed by 3-day SEDM culture. Transduced (GFP+) cells were purified by sorting and plated for colonies. Bars are representative of mean ± SEM. *P < .05; **P < .001; **P < .005; ****P < .0001.
The function of SelenoW in stress erythropoiesis was further elucidated in primary BM cells. We used BM cells from TgCas9-GFP mice that express Cas9 and GFP.41 SelenoW knockdown or control BM cells (supplemental Figure 5B) were cultured in the 2-phase culture system to estimate their ability to generate SEPs. We observed decreased cell expansion of mutant cells compared with control group during both expansion and differentiation culture (Figure 5F). There were fewer stress BFU-E colonies formed from mutant cells (Figure 5G), indicating that fewer SEPs were generated from BM cells in the absence of SelenoW. To rule out the effects of nontransduced cells, we sorted the cells after differentiation according to GFP and mCherry reporters. As expected, there was a significant reduction in the number of BFU-E colonies when equal numbers of GFP+mCherry+ (transduced) cells and GFP single positive (nontransduced) cells were plated (Figure 5H). We extended this analysis of SelenoW to human stress erythropoiesis. SELENOW expression in human BM cells was knocked down using a lentiviral vector expression dCas9-KRAB51 and gRNA specific for the promoter of human SELENOW. Using BM from 3 different donors, we observed that in each case, cultures infected with the sgRNA specific for SELENOW generated fewer colonies than their paired control infected culture. SELENOW sgRNA viruses reduced the expression SelenoW, as measured by quantitative reverse transcription polymerase chain reaction analysis (Figure 5I; supplemental Figure 5H). These data reinforce the observation made in the murine system and demonstrate a role for SelenoW in the regulation of the expansion of SEPs during stress erythropoiesis.
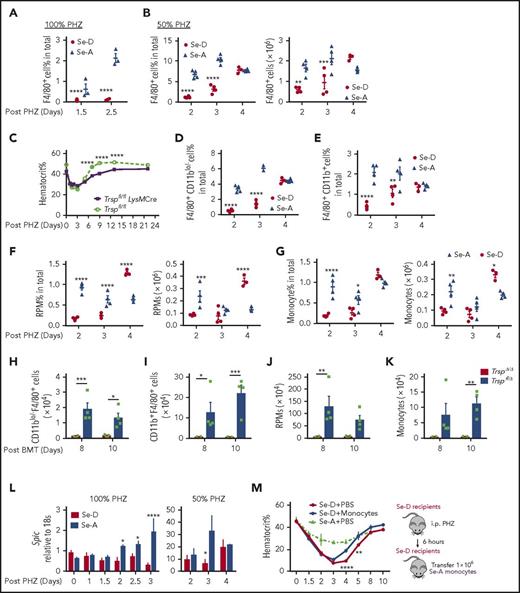
Se and selenoproteins deficiency impairs macrophages and monocytes during stress erythropoiesis
EBIs are specialized niches in which erythroblasts proliferate and mature. Macrophages within the EBI express Vcam-1, whose ligand is α4β1 on the erythroblasts.15,19,20 Splenic α4+CD71hiTer119+ cells are early erythroblasts with relatively larger cell size (supplemental Figure 6A). 100% PHZ-treated Se-D mice contained significantly fewer α4+ early erythroblasts, as well as decreased numbers of F4/80+ splenic macrophages, when compared with Se-A mice on days 1.5 and 2.5 (Figure 6A; supplemental Figure 6A-B). Similarly, 50% PHZ-treated mice exhibited a delayed expansion of splenic F4/80+ macrophages (Figure 6B; supplemental Figure 6C). When we deleted selenoproteins in cells of the myeloid lineage using Trspfl/flLysMCre, the mice exhibited a delayed recovery from anemia (Figure 6C). These data suggested Se status and selenoproteins affect macrophages in the niche, contributing to defects in stress erythropoiesis.
Absence of selenoproteins in macrophages and monocytes delays stress erythropoiesis. (A-B) Flow cytometry analysis of F4/80+ macrophages in the spleens of Se-A and Se-D mice treated with PHZ. (A) 100% PHZ treatment. Percentage F4/80+ cells were measured on the indicated days; n = 3 per diet. (B) 50% PHZ treatment. Percentage (left) and total numbers (right) of F4/80+ cells on indicated days after 50% PHZ treatment; n = 4 per diet. (C) Analysis of mice with deletion of Trsp in myeloid cells. Trspfl/flLysMCre mice were treated with 100% PHZ and hematocrit levels were measured on the indicated days after treatment; n = 3-4 per group. (D-G) Analysis of macrophage and monocyte populations in the spleens of Se-A and Se-D mice treated with 50% PHZ. (D-E) Flow cytometry analysis of (D) F4/80+CD11blo/− cells and (E) F4/80+CD11b+ cells; n = 4 per diet. (F) Flow cytometry analysis of spleen RPMs (F4/80+CD11blo/−Vcam1+) after 50% PHZ treatment. Percentage of RPMs (left) and total numbers (right); n = 4 per diet. (G) Flow cytometry analysis of CD11b+CD115+ monocytes in the spleen on the indicated days after 50% PHZ treatment. Percentage (left) and total numbers (right) of monocytes; n = 4 per diet. (H-K) Quantitation of monocyte and macrophage populations in the spleen of TrspΔ/Δ or control cells transplanted mice on days 8 and 10 after BMT; n = 4 per group. (H) F4/80+CD11blo/− cells, (I) F4/80+CD11b+ cells, (J) RPMs, (K) monocytes. (L) Analysis of Spic expression in the spleen on the indicated days after PHZ treatment by quantitative reverse transcription polymerase chain reaction. 100% PHZ (left; n = 3-7 per diet) and 50% PHZ (right; n = 3-4 per diet). (M) Rescue of Se-D defects in spleen macrophages by adoptive transfer of monocytes. CD11b+Ly6G− monocytes were isolated from spleens of Se-A mice by magnetic bead enrichment and injected into Se-D mice 6 hours after 50% PHZ treatment. Hematocrit values were measured as indicated; n = 3 for each group. Bars are representative of mean ± SEM. *P < .05; **P < .001; ***P < .005; ****P < .0001.
Absence of selenoproteins in macrophages and monocytes delays stress erythropoiesis. (A-B) Flow cytometry analysis of F4/80+ macrophages in the spleens of Se-A and Se-D mice treated with PHZ. (A) 100% PHZ treatment. Percentage F4/80+ cells were measured on the indicated days; n = 3 per diet. (B) 50% PHZ treatment. Percentage (left) and total numbers (right) of F4/80+ cells on indicated days after 50% PHZ treatment; n = 4 per diet. (C) Analysis of mice with deletion of Trsp in myeloid cells. Trspfl/flLysMCre mice were treated with 100% PHZ and hematocrit levels were measured on the indicated days after treatment; n = 3-4 per group. (D-G) Analysis of macrophage and monocyte populations in the spleens of Se-A and Se-D mice treated with 50% PHZ. (D-E) Flow cytometry analysis of (D) F4/80+CD11blo/− cells and (E) F4/80+CD11b+ cells; n = 4 per diet. (F) Flow cytometry analysis of spleen RPMs (F4/80+CD11blo/−Vcam1+) after 50% PHZ treatment. Percentage of RPMs (left) and total numbers (right); n = 4 per diet. (G) Flow cytometry analysis of CD11b+CD115+ monocytes in the spleen on the indicated days after 50% PHZ treatment. Percentage (left) and total numbers (right) of monocytes; n = 4 per diet. (H-K) Quantitation of monocyte and macrophage populations in the spleen of TrspΔ/Δ or control cells transplanted mice on days 8 and 10 after BMT; n = 4 per group. (H) F4/80+CD11blo/− cells, (I) F4/80+CD11b+ cells, (J) RPMs, (K) monocytes. (L) Analysis of Spic expression in the spleen on the indicated days after PHZ treatment by quantitative reverse transcription polymerase chain reaction. 100% PHZ (left; n = 3-7 per diet) and 50% PHZ (right; n = 3-4 per diet). (M) Rescue of Se-D defects in spleen macrophages by adoptive transfer of monocytes. CD11b+Ly6G− monocytes were isolated from spleens of Se-A mice by magnetic bead enrichment and injected into Se-D mice 6 hours after 50% PHZ treatment. Hematocrit values were measured as indicated; n = 3 for each group. Bars are representative of mean ± SEM. *P < .05; **P < .001; ***P < .005; ****P < .0001.
We further examined how selenoprotein deficiency affected macrophage populations in the spleen. Both CD11blo/−F4/80+ and CD11bhiF4/80+ cells were significantly decreased in the spleens of Se-D mice compared with the Se-A mice on days 2 and 3 after 50% PHZ treatment (Figure 6D-E; supplemental Figure 6D). In addition, there were significantly fewer RPMs (CD11blo/−Vcam-1+F4/80+) in the Se-D mice (Figure 6F; supplemental Figure 6E). CD11bhiCD115+ monocytes, which are the precursors of RPMs,29 were also significantly decreased (Figure 6G; supplemental Figure 6E). Similar results were observed in mice transplanted with TrspΔ/Δ BM cells on days 8 and 10 post-BMT (Figure 6H-K).
The development of RPMs requires the transcription factor SpiC.28-30 Unlike Se-A mice, Se-D mice failed to increase Spic expression during recovery from anemia (Figure 6L), indicating a defect in the maturation of RPMs from monocytes. This defect likely resulted in the reduction of RPMs observed in Se-D mice. Transfer of Se-A CD11b+ monocytes into 50% PHZ-treated Se-D mice significantly accelerated recovery from anemia when compared with phosphate-buffered saline-treated controls (Figure 6M), albeit at a lower recovery rate when compared with Se-A mice, suggesting that Se-A monocytes partially rescued the defective phenotype of Se-D mice.
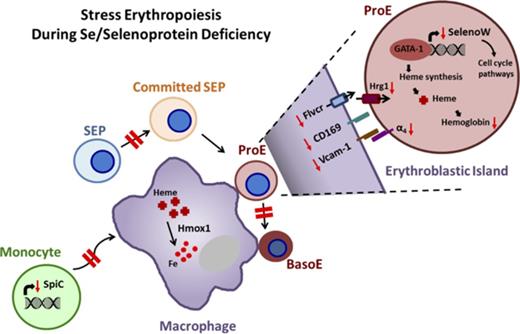
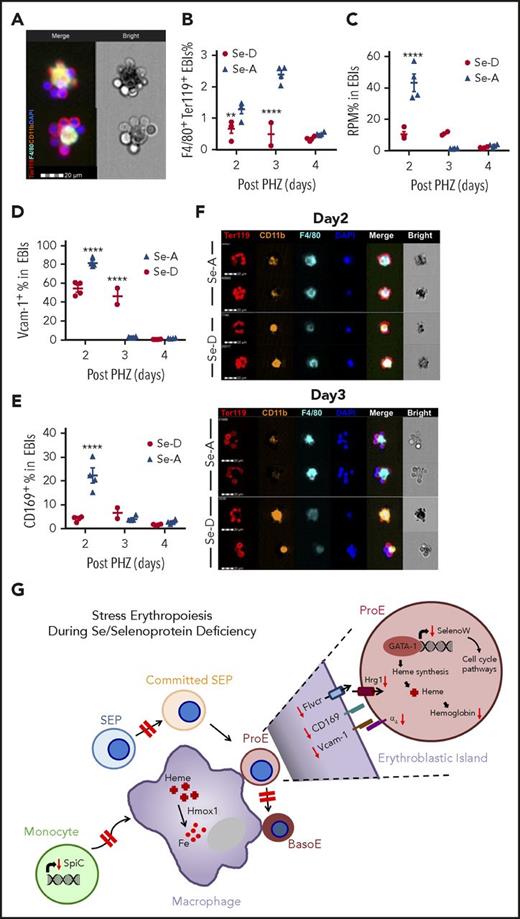
Impaired development of the stress erythropoietic microenvironment in Se-D mice
Splenic EBIs are marked by expression of Ter119 on erythroblasts and F4/80 on macrophages (Figure 7A). We observed significantly reduced splenic EBIs in Se-D mice compared with Se-A mice on days 2 and 3 after 50% PHZ treatment, with remarkably fewer RPMs in EBIs from Se-D mice (Figure 7B-C; supplemental Figure 7A). In addition, EBIs from Se-D mice exhibited a delayed upregulation of Vcam-1 and CD169 expression on EBI macrophages (Figure 7D-E; supplemental Figure 7B). Analysis using FlowSight Imaging flow cytometry further elucidated dynamics of EBI macrophages and erythroblasts. On day 2 after PHZ treatment, Ter119+ EBI macrophages in both Se-D and Se-A mice were CD11bhiF4/80hi, surrounded by enucleated erythroblasts that were terminally differentiated (Figure 7F). On day 3, EBI macrophages in Se-A exhibited RPM-like phenotype with downregulated CD11b expression surrounded by large nucleated early erythroblasts, indicating efficient erythropoiesis. However, EBI macrophages in the Se-D mice retained high CD11b expression, consistent with the idea of defective RPM formation. In addition, morphologically Se-D EBIs appeared less viable with fewer early erythroblasts attached (Figure 7F). Overall, these results depict an impaired erythropoietic niche under Se-deficient conditions, which is associated with defects in monocytes and macrophages. Taken together, our results suggest that Se and selenoproteins are important for the development of not only erythroid progenitors but the microenvironment as well (Figure 7G).
Defective EBI formation in Se-D mice is partially responsible for the ineffective stress erythropoiesis. (A) Representative picture of spleen EBI structure. EBIs are Ter119+F4/80+ aggregates. (B) Flow cytometry analysis of EBIs on the indicated days after 50% PHZ treatment; n = 2-4 per diet. Two independent experiments. (C) Flow cytometry analysis of RPMs in EBIs on the indicated days after 50% PHZ treatment; n = 2-4. (D-E) Flow cytometry analysis of (D) Vcam-1 and (E) CD169 expression on EBI macrophages on the indicated days after 50% PHZ treatment; n = 2-4 per diet. (F) Representative FlowSight analysis of EBIs at day 2 and day 3 after 50% PHZ treatment. Four independent experiments. Bars are representative of mean ± SEM. (G) Schematic representation of ineffective stress erythropoiesis during Se and selenoprotein deficiency. Red dashed arrows indicate the process is delayed or impaired. Red solid arrows indicate downregulation or decreased level of the molecules. In the normal condition, in response to stress, SEPs and erythroid precursors rapidly expand and differentiate. SelenoW expression is upregulated in the erythroblasts by GATA-1, regulating cell cycle and hemoglobin synthesis. Increased number of RPMs mature from monocytes, expanding the erythropoietic niche to support erythroblast maturation. Adhesion molecules are upregulated in the EBIs, as well as heme biosynthesis-related genes and pathways to bolster the process. However, in the absence of Se or selenoproteins, SEP expansion and differentiation is delayed. Erythroblast maturation in the niche is less efficient because of the deficits in both erythroblasts and macrophages. Heme homeostasis is perturbed, resulting in improper downstream signaling. **P < .001; ****P < .0001.
Defective EBI formation in Se-D mice is partially responsible for the ineffective stress erythropoiesis. (A) Representative picture of spleen EBI structure. EBIs are Ter119+F4/80+ aggregates. (B) Flow cytometry analysis of EBIs on the indicated days after 50% PHZ treatment; n = 2-4 per diet. Two independent experiments. (C) Flow cytometry analysis of RPMs in EBIs on the indicated days after 50% PHZ treatment; n = 2-4. (D-E) Flow cytometry analysis of (D) Vcam-1 and (E) CD169 expression on EBI macrophages on the indicated days after 50% PHZ treatment; n = 2-4 per diet. (F) Representative FlowSight analysis of EBIs at day 2 and day 3 after 50% PHZ treatment. Four independent experiments. Bars are representative of mean ± SEM. (G) Schematic representation of ineffective stress erythropoiesis during Se and selenoprotein deficiency. Red dashed arrows indicate the process is delayed or impaired. Red solid arrows indicate downregulation or decreased level of the molecules. In the normal condition, in response to stress, SEPs and erythroid precursors rapidly expand and differentiate. SelenoW expression is upregulated in the erythroblasts by GATA-1, regulating cell cycle and hemoglobin synthesis. Increased number of RPMs mature from monocytes, expanding the erythropoietic niche to support erythroblast maturation. Adhesion molecules are upregulated in the EBIs, as well as heme biosynthesis-related genes and pathways to bolster the process. However, in the absence of Se or selenoproteins, SEP expansion and differentiation is delayed. Erythroblast maturation in the niche is less efficient because of the deficits in both erythroblasts and macrophages. Heme homeostasis is perturbed, resulting in improper downstream signaling. **P < .001; ****P < .0001.
Discussion
Our data demonstrate a key role for selenoproteins in the early SEP expansion in the spleen. Lack of selenoproteins in Trsp mice blocked the development of these SEPs in culture. This defect was further underscored when Trsp-deleted BM cells failed to provide erythroid short-term radioprotection after transplantation. Mutation of SelenoW, which was the most highly regulated selenoprotein in the splenic ProEs as a function of Se-status during stress, resulted in a partial defect in the expansion of early SEPs, suggesting SelenoW is involved in this regulation. SelenoW has been shown to positively regulate the Hippo pathway-regulated transcription factor Taz during muscle cell differentiation by inhibiting 14-3-3-mediated Taz cytoplasmic translocation and sequestration.49 The hippo pathway regulates organ size by inhibiting the action of Taz and a related factor Yap1.52 We observed that there was a higher ratio of cytoplasmic over nuclear Yap1 of BM cells in the absence of SelenoW grown in SEDM culture that was not seen when cells were grown in SEEM culture (supplemental Figure 8), suggesting that SelenoW may mediate differentiation of SEPs by regulating Yap1 translocation via 14-3-3.
In addition to the defect in SEP expansion, we observed a striking reduction in splenic EBIs in Se-D mice coupled with decreased α4+CD71+ early erythroblasts. In addition, Se-D mice failed to expand RPMs. Although RPMs are tissue-resident macrophages, new RPMs can be replenished from monocytes that develop through a pre-RPM (CD11bhiF480+) intermediate stage.30 Under Se adequate conditions, where all the selenoproteins are expressed, pre-RPMs initially present within the EBIs associated with erythrocytes; later stages show increased numbers of mature RPMs associated with early erythroblasts, suggesting erythroblasts and central macrophages could mature simultaneously. However, in Se-D mice, mature RPMs were rarely observed in EBIs. In contrast, Pre-RPMs were the major cells associated with Se-D EBIs. This observation raises a potential issue with EBI integrity, as expression of Vcam-1 and CD169 is reduced on immature RPMs, and the upregulation of their expression is delayed in Se-D mice. The delay could potentially affect their interaction with the developing erythroblasts. Deletion of Trsp using the myeloid-specific LysMCre results in a delayed the recovery of mice from PHZ-induced anemia, which further supports this model.
The transcription factor SpiC regulates the development of RPMs from monocytes, which is induced by heme-dependent signaling.29 In Se-D mice, Bach1 expression remained high and Spic expression was not upregulated (Figure 6L), indicating low cellular heme. Consistent with this idea, Se-D mice expressed lower levels of heme transporter Hrg1,53 heme exporter Flvcr1,54 and heme oxygenase Hmox155 in EBIs (supplemental Figure 7D-G), suggesting defects in heme transport and homeostasis. In contrast, Se-D ProEs expressed more Hrg1 than Se-A ProEs (supplemental Figure 7H), suggesting the defect in Hrg1 expression was limited to the EBI macrophages. The increased Hrg1 expression in ProEs may be a compensatory response for the lack of heme transport from EBI macrophages. Taken together, these results suggest that abnormal heme homeostasis in the EBIs under Se-D conditions could be a contributor to ineffective erythroid terminal maturation, pointing to critical role of selenoproteins in the expansion and development of SEPs, as well as the erythroid niche during recovery from acute anemia (Figure 7G). In summary, diet-induced Se deficiency or genetic deletion of the selenoproteome severely compromises stress erythropoiesis to negatively affect expansion of early SEPs and maturation of erythroblasts that is also associated with defective EBIs. Our data also suggest an important role for SelenoW, which regulates the proliferation of stress BFU-Es in addition to the transition from ProEs to BasoEs. Thus, selenoproteins are required for efficient stress erythropoiesis at multiple levels.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank members of the K.S.P. and R.F.P. laboratories for their timely help and suggestions and the Flow Cytometry Core Facility at Penn State University. pLV hU6-sgRNA hUbC-dCas9-KRAB-T2a-GFP was a gift from Charles Gersbach (Addgene plasmid 71237).
This work was supported, in part, by grants from the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK077152 [K.S.P.] and R01 DK080040 [R.F.P.]), Office of Dietary Supplements (K.S.P.), and US Department of Agriculture–National Institute of Food and Agriculture Hatch project numbers 4605 (K.S.P) and 4581 (R.F.P).
Authorship
Contribution: C.L. performed experiments and wrote the manuscript; R.C.H. and M.J.K. provided expertise and feedback; R.C.H. and B.A.C. provided resources and assisted in manuscript preparation; and R.F.P. and K.S.P. supervised and conceived the study, secured funds, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: K. Sandeep Prabhu, Department of Veterinary and Biomedical Sciences, Pennsylvania State University, 115 Henning Building, Shortlidge Rd, University Park, PA 16802; e-mail: ksp4@psu.edu; and Robert F. Paulson, Department of Veterinary and Biomedical Sciences, Pennsylvania State University, 115 Henning Building, Shortlidge Rd, University Park, PA 16802; e-mail: rfp5@psu.edu.

![Figure 1. Se deficiency impairs stress erythropoiesis after PHZ administration. (A) Schematic of the study model. C57BL/6 mice were fed on a Se-D or Se-A diet for 12 weeks before use. Then mice were treated with PHZ (100 mg/kg [100%] or 50 mg/kg [50%]). Kinetics of stress erythropoiesis were evaluated by time course study. (B-G) Kinetics of stress erythropoietic recovery of Se-D and Se-A mice treated with 100% PHZ. (B) Survival curve of mice over the course of 12 days of recovery; n = 8 per diet. (C) Hematocrit measurements of mice during the recovery from PHZ-induced anemia; n = 10-15 per diet. (D) Normalized reticulocyte percentage in the whole blood at days 1.5 and 2.5 after PHZ treatment; n = 3 per diet. (E) Spleen weights (left) and the representative pictures of spleens (right) from mice on the different diets on the indicated days after PHZ treatment; n = 3-7 per diet. (F) Hematoxylin and eosin staining of spleen sections from Se-D and Se-A mice on the indicated days after PHZ treatment (original magnification ×100). (G) Stress BFU-E colony assays of spleen cells isolated from Se-D and Se-A mice at indicated times after PHZ treatment (left) and representative pictures of BFU-E colony morphology on day 3 posttreatment (right; acid benzidine stain; original magnification ×50); n = 3-6 per diet. Bars are representative of mean ± SEM. **P < .001; ***P < .005; ****P < .0001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/131/23/10.1182_blood-2017-08-800607/4/m_blood800607f1.jpeg?Expires=1765905293&Signature=k~b9vUkkQEzmfW6yOQTq3E-2KGiX3JBbLq1nT6ioXJ7IZIwyrd4rY-Vf0KOSHI2HdiUroVWjAX0X1b4szOBGNFHkoTjxbrSS6NuglW5qvYddAxjjaXPjcEQNuRPQWpc771ofu5NccyRjJD6MsLeVeGAeHMv5nEv9GRmWuL-HxWfGNcl1cb3-6~yiBd54TsqCzxmFQrsiUufyxL4RqOOrGosUFxLcrzbqZbatTmQ9vYdoSu-qD9vALoz0dTXBmGeJFegQ8WTmtEtf~aBe7JK~JJSEAPDOx8zgXGNSFuxJ40buv0U5-stI2CDzf8V0TXS6PvERtfZv4qJwB5qTTzgSQA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 2. Se and selenoproteins are required in early SEPs. (A-D) Analysis of Se-A and Se-D mice treated with 50% PHZ. (A) Survival of Se-A and Se-D mice treated with 50% PHZ; n = 8 per diet. (B) Analysis of hematocrit during recovery from treatment with 50% PHZ; n = 10-15 per diet. (C) Representative flow cytometry graphs of Kit+CD133+early SEPs during recovery from PHZ treatment. (D) Quantitation of spleen Kit+CD133+early SEPs and Kit single-positive cells during recovery; n = 3-4 per diet. (E-F) In vitro analysis of TrspΔ/Δ and control cells using 2-phase stress erythropoiesis culture; n = 4 per group. (E) Total cell numbers postexpansion culture (in stress erythropoiesis expansion medium [SEEM]) and differentiation culture (in stress erythropoiesis differentiation medium [SEDM]). (F) Stress BFU-E colony assays of cells after differentiation culture. (G-J) In vivo short-term radioprotective model. Donor BM cells were obtained from Trspfl/Δ;CreERT or control Trspfl/Δ mice. Trsp gene deletion was induced by treating cells with 4-hydroxytamoxifen in vitro 48 hours before bone marrow transplant. (G) Survival rate and (H) hematocrit measurements of transplanted mice on the indicated days posttransplant. Two independent repeats; n = 5 for each group. (I) Total spleen SEPs on days 8 and 10 after BMT; n = 4 per group. (J) Stress BFU-E colony assays of spleen cells on day 10 after BMT; n = 4 per group. Bars are representative of mean ± SEM. *P < .05; ***P < .005; ****P < .0001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/131/23/10.1182_blood-2017-08-800607/4/m_blood800607f2.jpeg?Expires=1765905293&Signature=vIxosxx12-h9cDPUDC~nTY1Nyo1-il5l8ofLR7mgpeDYKCiGect-DApD-VVwpUcFryfsylkt99M2RYtRCa-1IX~71Hat-3tlyn8YmjqqyAwxXhqq5K6sBafIDIiu6lIFxrpcCeem~H0Hm9WJrPPCzsx9cMP4Pi8hHTBAYeEifH~Q1qfRpKMU~65E4xlxuPCo1E4DnrhKXWNDvYMk0JcoMs~Z5KQfxEAnLQQkUpLUFNWEWwH--a1TTo4ya6CkN0c2A1dG24iMyAnpc202SouNt3cV8bOgJL3TXiR7-cmGaWcjAFpOtVeNrSyg8l6L5Il6wWh0-OFY6HB65Qc2klsFZg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal