In this issue of Blood, Rowczenio et al investigate the role of genetic factors, inflammasome activation, and proinflammatory cytokines in the pathogenesis of Schnitzler syndrome.1
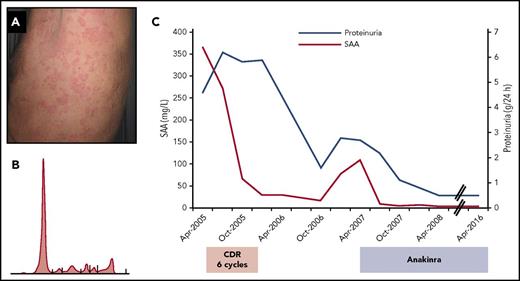
Clinical presentation and course of a patient with Schnitzler syndrome and reactive AA amyloidosis treated with anticlone therapy followed by IL-1 blocking treatment. A 55-year-old man was diagnosed with amyloidosis by renal biopsy. (A) During the previous 30 years, he had chronic nonpruritic urticarial rash associated with recurrent fever (up to 39°C) and arthralgia. Proteinuria and subsequent nephrotic syndrome were associated with profound postural hypotension and diarrhea. (B) A small (8 g/L) IgMκ monoclonal protein was detected with a 6% clonal bone marrow lymphoplasmacytic infiltrate. Proteinuria was 4.6 g per 24 hours, and there were no signs of amyloid cardiac or liver involvement. Amyloid deposits were detected in the abdominal fat, which reacted with anti-serum amyloid A (anti-SAA) apolipoprotein antibodies and not with anti-κ and anti-λ light chain antibodies. (C) A diagnosis of AA amyloidosis due to Schnitzler syndrome with kidney and autonomic nervous system involvement was made, and the patient was treated with cyclophosphamide, rituximab, and dexamethasone, with improvement of clinical symptoms and reduction of SAA and proteinuria. After 18 months, an increase in SAA and proteinuria accompanied an exacerbation of symptoms, and the patient was placed on anakinra, resulting in complete clinical remission and normalization of SAA and proteinuria. Apr, April; CDR, cyclophosphamide, rituximab, and dexamethasone; Oct, October; SAA, serum amyloid A.
Clinical presentation and course of a patient with Schnitzler syndrome and reactive AA amyloidosis treated with anticlone therapy followed by IL-1 blocking treatment. A 55-year-old man was diagnosed with amyloidosis by renal biopsy. (A) During the previous 30 years, he had chronic nonpruritic urticarial rash associated with recurrent fever (up to 39°C) and arthralgia. Proteinuria and subsequent nephrotic syndrome were associated with profound postural hypotension and diarrhea. (B) A small (8 g/L) IgMκ monoclonal protein was detected with a 6% clonal bone marrow lymphoplasmacytic infiltrate. Proteinuria was 4.6 g per 24 hours, and there were no signs of amyloid cardiac or liver involvement. Amyloid deposits were detected in the abdominal fat, which reacted with anti-serum amyloid A (anti-SAA) apolipoprotein antibodies and not with anti-κ and anti-λ light chain antibodies. (C) A diagnosis of AA amyloidosis due to Schnitzler syndrome with kidney and autonomic nervous system involvement was made, and the patient was treated with cyclophosphamide, rituximab, and dexamethasone, with improvement of clinical symptoms and reduction of SAA and proteinuria. After 18 months, an increase in SAA and proteinuria accompanied an exacerbation of symptoms, and the patient was placed on anakinra, resulting in complete clinical remission and normalization of SAA and proteinuria. Apr, April; CDR, cyclophosphamide, rituximab, and dexamethasone; Oct, October; SAA, serum amyloid A.
Schnitzler syndrome is a rare disorder characterized by recurrent or chronic urticaria associated with a monoclonal gammopathy and persistent inflammation.2 This disorder often goes undiagnosed.3 The rash is typically resistant to antihistamines, and histologically, it is a neutrophilic urticarial dermatosis. The monoclonal protein is an immunoglobulin Mκ (IgMκ) in 80% to 90% of cases. In the remaining patients, IgMλ and IgG monoclonal proteins have been reported. The invariable presence of the monoclonal protein suggests a possible pathogenic role, which has remained elusive. Additional features, which are minor diagnostic criteria, include intermittent fever, arthralgia, bone pain, liver or spleen enlargement, palpable adenopathy, elevated markers of inflammation, and bone abnormalities on radiological investigations. Fatigue is frequent, and the clinical manifestations are often disabling. Schnitzler syndrome can progress to Waldenström macroglobulinemia or other lymphoproliferative disorders, with a frequency comparable to that of patients with IgM monoclonal gammopathy of undetermined significance. Moreover, systemic amyloid A (AA) amyloidosis that occurs as a consequence of chronic inflammation may develop (see figure). To prevent this, treatment should be aimed at reducing the concentration of serum amyloid A apolipoprotein, even in patients with moderate or controlled symptoms. Light chain amyloidosis is a theoretical possibility, although no cases have been reported so far.
Inflammation and proinflammatory cytokines, particularly interleukin-1β (IL-1β), play a key role in the pathogenesis of Schnitzler syndrome, and treatment with the IL-1 receptor antagonist anakinra results in complete control of symptoms in more than 80% of patients.4 Other IL-1 blocking approaches, such as canakinumab, an anti-IL-1β antibody, and rilonacept, a fusion protein consisting of the ligand-binding domains of IL-1 receptor and IL-1 receptor accessory protein fused to the Fc region of human IgG1 that binds and neutralizes IL-1, have shown promising activity.2 Although IL-1 blocking therapy dramatically improves quality of life, it is not curative and probably does not prevent the development of lymphoproliferative disorders. Schnitzler syndrome apparently is an acquired autoinflammatory disease. Autoinflammatory diseases, an ever-expanding universe, are caused by acquired or hereditary dysregulation of the innate immune system. The hereditary disorders are caused by many mechanisms, including inappropriate inflammasome-mediated production of the cytokine IL-1β and perturbations in signaling by the transcription nuclear factor κB, ubiquitination, cytokine signaling, and protein folding.5 Although it can be discriminated on a clinical basis,6 the presentation of Schnitzler syndrome is very similar to that of the hereditary autoinflammatory disease cryopyrin-associated periodic syndromes (CAPS). This condition is caused by activating mutations in the NLRP3 gene (nucleotide-binding oligomerization domain-leucine-rich repeats containing pyrin domain 3). Indeed, the common variant NLRP3p.V198M was found in 2 patients with classical (IgM) Schnitzler syndrome, and somatic NLRP3 mosaicism was identified in the myeloid lineage of 2 patients with variant (IgG) Schnitzler syndrome. On the basis of these findings, Rowczenio and colleagues performed a next-generation sequencing-based search for mutations in NLRP3 and 32 other genes associated with monogenic autoinflammatory diseases in 21 patients with Schnitzler syndrome. Their search confirmed the presence of the NLRP3p.V198M variant in 1 patient that was previously reported, but no additional predisposing abnormalities in NLRP3 or in the other 32 targeted genes were detected. However, Rowczenio and colleagues found higher levels of apoptosis-associated speck-like protein with Card domain aggregates, IL-6, and IL-18 in the sera of their 21 patients, in comparison with controls, which were similar to levels measured in CAPS patients. This clearly indicates the activation of inflammasome. However, the mechanism of this activation remains obscure. The authors report a series of rare allele variants in the 32 targeted genes, some of which are listed in the registry of hereditary autoinflammatory disorders mutations, but their clinical significance is currently unknown. Future studies will elucidate the possible role of genetic factors in Schnitzler syndrome.
The interplay between the lymphoplasmacytic clone and the activation of the inflammasome remains elusive, and it is possible that different manifestations can have different causes. For example, high levels of vascular endothelial growth factor, which decrease in successfully treated patients, and markers of bone formation, such as osteocalcin and bone-specific alkaline phosphatase, can underlie or reflect bone alterations.7 Also, it has been speculated that IL-1 stimulation may facilitate the onset of the lymphoplasmacytic clone through interactions between IL-1 receptor complex and IL-1 receptor-associated kinase with MYD88.2 The rarity of Schnitzler syndrome makes it extremely difficult to conduct large studies in this disorder, and international collaboration is crucial. However, the elucidation of the complex mechanisms underlying this fascinating disease may shed light on other autoinflammatory disorders and rare monoclonal gammopathies of clinical significance.
Conflict-of-interest disclosure: G.P. received honoraria from Janssen-Cilag, honoraria and travel support from Prothena, and travel support from Celgene. G.M. is a consultant for Millennium Pharmaceuticals, Inc., Pfizer, Janssen, Prothena, and IONIS.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal