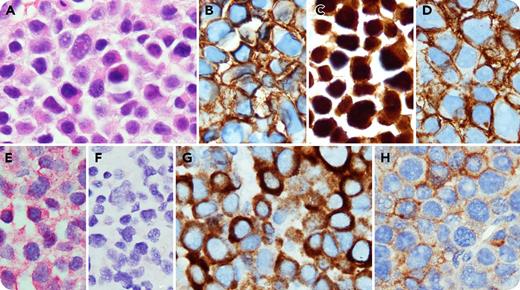
A 76-year-old woman presented with a lytic lesion involving the right ilium. A targeted biopsy showed diffuse infiltrate of atypical, pleomorphic plasma cells (panel A; original magnification ×1000, hematoxylin and eosin stain), positive for CD138 (panel B; original magnification ×1000), MUM1 (panel C; original magnification ×1000), CD56 (panel D; original magnification ×1000), cyclin D1 and λ (panel E; original magnification ×1000), and negative for CD19, CD20, CD117, κ (panel F; original magnification ×1000), and Epstein-Barr virus (EBV). The findings were diagnostic of a plasma cell neoplasm (PCN). Interestingly, the neoplastic cells showed strong cytoplasmic CD3ε (specific for the ε-chain of the human CD3) and dim CD4 expression (panels G-H; original magnification ×1000). Flow cytometry failed to detect the plasma cells. No other T-cell markers (CD2, CD5, CD7, or CD8) were detected. Serum and urine electrophoresis detected monoclonal immunoglobulin G-λ protein. The bone marrow showed no evidence of a PCN.
Aberrant T-cell antigen expression can be seen in various types of B-cell lymphoma. PCN can show aberrant antigen expression of different lineages, but expression of T-cell–related antigens, particularly dual CD3 and CD4, is exceedingly rare. Multiple theories have been proposed to explain the pathobiology of this phenomemon, including EBV infection, lineage infidelity, and Pax5 downregulation; however, the exact mechanism and clinical significance are still unclear. Nevertheless, this case emphasizes the importance of recognizing atypical and variable immunophenotypic aberrancies in PCN, which potentially could lead to diagnostic pitfalls.
A 76-year-old woman presented with a lytic lesion involving the right ilium. A targeted biopsy showed diffuse infiltrate of atypical, pleomorphic plasma cells (panel A; original magnification ×1000, hematoxylin and eosin stain), positive for CD138 (panel B; original magnification ×1000), MUM1 (panel C; original magnification ×1000), CD56 (panel D; original magnification ×1000), cyclin D1 and λ (panel E; original magnification ×1000), and negative for CD19, CD20, CD117, κ (panel F; original magnification ×1000), and Epstein-Barr virus (EBV). The findings were diagnostic of a plasma cell neoplasm (PCN). Interestingly, the neoplastic cells showed strong cytoplasmic CD3ε (specific for the ε-chain of the human CD3) and dim CD4 expression (panels G-H; original magnification ×1000). Flow cytometry failed to detect the plasma cells. No other T-cell markers (CD2, CD5, CD7, or CD8) were detected. Serum and urine electrophoresis detected monoclonal immunoglobulin G-λ protein. The bone marrow showed no evidence of a PCN.
Aberrant T-cell antigen expression can be seen in various types of B-cell lymphoma. PCN can show aberrant antigen expression of different lineages, but expression of T-cell–related antigens, particularly dual CD3 and CD4, is exceedingly rare. Multiple theories have been proposed to explain the pathobiology of this phenomemon, including EBV infection, lineage infidelity, and Pax5 downregulation; however, the exact mechanism and clinical significance are still unclear. Nevertheless, this case emphasizes the importance of recognizing atypical and variable immunophenotypic aberrancies in PCN, which potentially could lead to diagnostic pitfalls.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal