Abstract
Venous thromboembolism (VTE) occurs at a higher rate in cancer patients and is frequently associated with well-known prothrombotic risk factors such as prolonged bed rest, central venous catheters, diverse oncological treatments and invasive procedures. Patients may share one or more risk factors. In addition, there seem to be tumor-driven prothrombotic pathways. Thus different tumors may promote activation of coagulation either directly through the expression of procoagulant molecules such as tissue factor or indirectly through the secretion of factors that in turn induce thrombocytosis or leukocytosis. Certain pathways may be more characteristic of a particular cancer cell type. Figuring out what these pathways are in different tumors may help better understand how these risk factors may be targeted.
Regarding ovarian cancer, it has been suggested that tumor-driven elevated platelet counts may be the pathway promoting thrombosis (Hisada Y and Mackman N. Blood 2017 :blood-2017-03-743211). Indeed platelet counts above 450,000/ul are reported in close to a third of women with ovarian cancer at diagnosis and murine models show aberrant IL-6/IL-6R expression by malignant cells which induce hepatic thrombopoietin secretion driving thrombocytosis (Stone RL et al N Engl J Med. 2012, 16;366(7):610-8) In fact, high IL-6 levels have been documented in woman with ovarian cancer. Another pathway is tumor-induced leucocytosis through expression of granulocyte colony stimulating factor (G-CSF) by ovarian cancer cells. Broad G-CSF and GCSF receptor expression has been reported across all ovarian cancer primary cell lines. Despite these observations, to our knowledge there are no reports showing that high platelet and/or leukocyte counts indeed correlate with VTE.
We sought to evaluate the incidence and prognostic impact of VTE in women with an initial diagnosis of ovarian cancer as well as the prevalence and impact of thrombocytosis or leukocytosis on the incidence of VTE and on survival. We retrospectively looked at a cohort of women with epithelial ovarian cancer admitted at the NCI in Mexico between Jan-Nov 2017. Baseline pretreatment complete blood counts were obtained in 118 consecutive women (mean age 53; 19 - 82 years). We obtained pathological staging data, doppler US and CT images were reviewed for corroboration of extent of VTE. Standard statistical analysis was carried out using SPSS software version 20 (SPSS Inc., Chicago, IL).
With a median follow up of 6.5 months (range: 0.5 - 13.7) the incidence of VTE was 13.4% (n=16). Consistent with other reports, patients often developed VTE at diagnosis 44% (n=7/16) associated with tumor activity before having been subjected to treatment. Six women developed VTE in association with surgery (mean of 24.6 days post-operatively; range 4- 58). The other 3 developed VTE in association with neoadjuvant chemotherapy (without surgery). As compared to patients with serous carcinoma, those with endometrioid carcinoma had a higher risk of VTE (8/91: 8.8%; 4/9: 44.4%, respectively, p<0.001) yet the number of patients with endometriod carcinoma is small. Women with VTE showed a trend to having a more advanced TNM stage at diagnosis, stage IV (44.7% vs 75%; p=0.083).
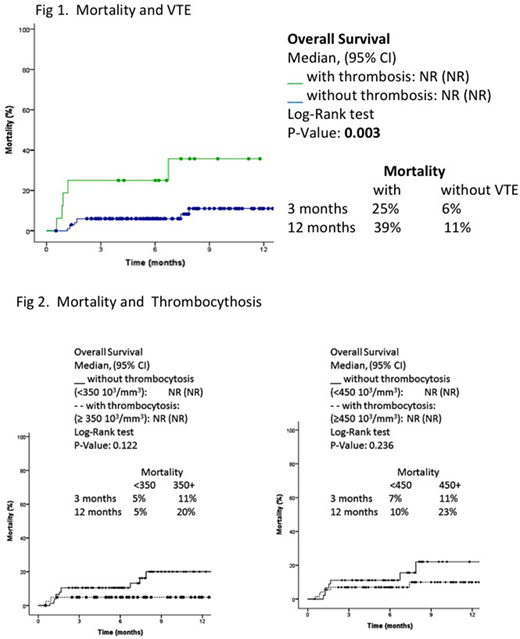
Despite a high prevalence of thrombocytosis 37.8% (n=45) using cutoff values of >350x 103/□l or 450 x 103/□l. this was not a risk factor for symptomatic thrombosis in our patients. The median platelet counts for all patients were 379 x 103/□l (range 31 - 914 x 103/□l), with no differences in patients with or without VTE: 407x 103/□l (107 - 914 x103/□l) and 378 103/□l (31 - 792 x103/□l) p=0.779, respectively. Notably, pretreatment leukocytosis, neutrophilia and monocytosis were all found to be associated with VTE. Women with VTE had higher median leukocyte counts (8.9 [4.5 - 27.3] vs 7.3 [3.1 - 29.3] 103/□l, p=0.051). Median neutrophyl counts were higher in VTE patients (6.5[3.2 - 23.6] vs. 5.1[1.8 vs.27.4] 103/mm3, p=0.036). Likewise, median monocyte count was higher among VTE patients (0.7 [0.3 - 1.7] vs. 0.5[0.3 - 1.2], p=0.042). Although mortality data is still premature, VTE was associated with a higher mortality rate at both six (27% vs 7%), and at 12 months (40% vs 13.4%; p:0.003) Fig 1. Thrombocytosis did not correlate with survival Fig 2. Thus leukocytosis, but not thrombocytosis, may constitute a prothrombotic pathway in women with ovarian cancer.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal