Abstract
Introduction:
Central Nervous System (CNS) involvement in multiple myeloma (MM) is a rare extramedullary manifestation which occurs in less than 1% of MM cases. The median survival after the diagnosis (Dx) is 1-2 months (M). Literature review revealed us of various treatment modalities i.e. systemic chemotherapy (CT), intrathecal therapy (IT), and radiotherapy (RT). The primary aim of our analysis is to summarize published literature on presentation patterns and review effective management strategies regarding CNS involvement in MM and its outcome.
Methods:
We performed a systematic review of 2533 articles published from 2005 using five databases (PubMed, Embase, Cochrane Library, Web of Science and ClinicalTrials.gov). After a detailed screening, 28 studies were included.
Results:
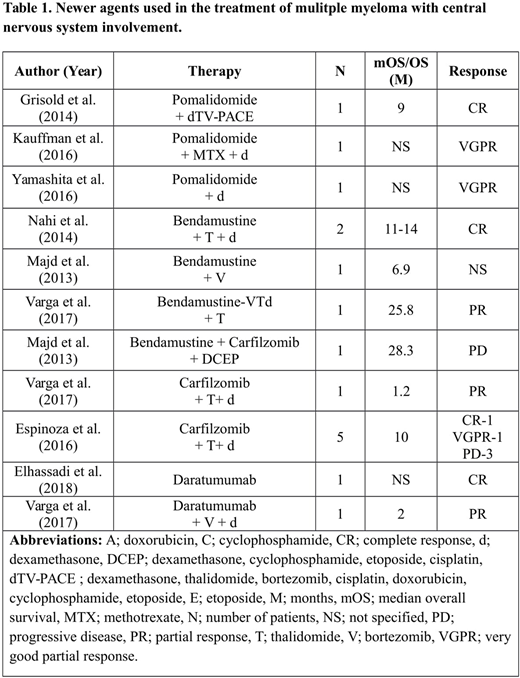
A total of 550 patients (pts) data is included. Eighty-eight (16%) pts had CNS involvement at the time of their initial presentation and 462 (84%) pts had disease detected at the time of relapse / refractory (R/R) disease . The median reported follow up, from the time of initial Dx, was 18 months (M) [range (r) = 3.4-75M]. The median age of pts was 58 years (y) (r= 40-71). The clinical presentations were heterogeneous with cranial nerve palsy (21%), headache (17%), confusion (17%), visual disturbances (17%), extremity weakness (9%), cord symptoms (5%) and nausea / vomiting (5%). The CNS region involved was identified in 366 pts: 163 (44.5%) pts had leptomeningeal (LM) involvement, 98 (26.8%) pts had dural (D)/osteodural (OD) involvement, 10 (2.7%) pts had LM + D/OD involvement, 90 (24.6%) pts had intraparenchymal (IP) involvement and 5 (1.4%) pts had LM + IP involvement. Hundred twenty-nine pts had International Staging System (ISS) information availabe at the time of MM Dx, out of which 39 (30%) pts had stage I disease, 32 (25%) pts had stage II disease and 58(45%) pts had stage III disease. The median time ( reported in studies) for CNS involvement after MM Dx ranges from 2.5-122 M in pts who underwent systemic treatment and 7-96 M in patients who underwent stem cell transplant (SCT). Five hundred twelve (93%) pts underwent treatment, out of which 42 (8.2%) pts had IT therapy with methotrexate and/or cytarabine, 44 (8.5%) pts had RT, 170 (33.2%) pts had CT, 103 (20.1%) pts had IT + RT + CT, 77 (15%) pts had RT + CT, 16 (3.1%) pts had IT + RT and 60 (11.7%) pts had IT + CT. One hundred two pts had SCT along with the other therapies. Among the pts who received systemic treatment, 34 patients received therapy with conventional agents (CA), 80 patients received therapy with novel agents (NA), 347 patients were treated with combination therapy of CA and NA. Data regarding the rest 51 patients were not available. Bortezomib (V) based regimens were given in 158 pts; immune-modulators (IMiD) based regimens in 153 pts; vincristine, adriamycin, dexamethasone (VAd) regimen in 21 pts; alkylators in 85 pts; carfilzomib in 7 pts; bendamustine in 5 pts; pomalidomide in 5 pts and daratumumab was given in 2 pts. The mOS in patients who received NA therapy was 4-25 M. The mOS in patients who received CA therapy was 2.7-8 M. The mOS in patients who received both CA and NA was 2-7.4 M. Seventy-five out of 512 patients were evaluated for efficacy, out of which, 30 pts showed complete response (CR), 6 pts showed very good partial response (VGPR), 17 pts showed partial response (PR) and progressive disease (PD) was seen in 22 pts. Death was reported in 370 out of total 550 pts.
Conclusion:
Our analysis demonstrated that systemic CT with CA & NA, RT and IT therapy either alone or in combination are the currently available strategies employed in treating CNS myeloma. Furthermore, NA therapies have shown an increase in the overall survival i.e. up to 25 months. The IMiD have shown good CNS penetrance [thalidomide (30-40%), lenalidomide (11%) and pomalidomide (39-49%)] and effectiveness in the clearance of myeloma cells from CSF. There is no established standard of care for CNS myeloma. As prognosis remain dismal for such patients, newer innovative approaches need to be tested in clinical trials (use of drugs like thiotepa, IT Daratumomab, combination regimens for IT therapy coupled with CNS penetrating systemic therapy etc.) to improve current treatment outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal