Abstract
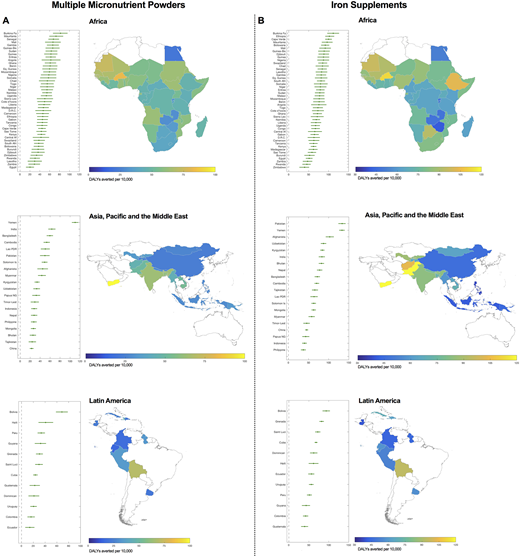
Almost 300 million children worldwide are anemic. Universal distribution of iron interventions (iron supplements or iron-containing multiple micronutrient powders, MNPs) to young children (e.g. <2 years of age) is a key World Health Organization recommendation to prevent anemia in low-income countries. However, concerns of iron-induced infection risk and limited effectiveness for anemia and broader child health outcomes have raised questions about whether iron interventions produce a net health benefit and are cost-effective. This has constrained implementation. Net effects likely differ in each country according to the epidemiology of anemia and infection, and local health care costs. Quality of implementation likely also affects net benefit. This means analyses must be country-specific. To help guide policymakers, we estimated country-specific net benefit-risk and cost-effectiveness of universal intervention with MNPs or iron supplements to young children. We developed a bespoke microsimulation model to estimate country-specific net Disability Adjusted Life Years (DALYs) attributable to anemia and infection in children from age 0-18 months who received MNPs, iron supplements or control from age 6-12 months. The model utilised publically available data on anemia, malaria, diarrhoea and respiratory infection epidemiology, and modified their risks according to effect sizes from the pivotal systematic reviews of randomised trials used to inform current guidelines. We next estimated corresponding cost/ DALY averted. We modeled all 78 countries (46 in Africa, 20 in Asia and 12 in Latin America) where WHO reported that anemia prevalence exceeded 40% in 2011, or where pilot iron intervention programmes have been reported to be in place. We found that MNPs and iron supplements produced a net benefit to health in all countries, though the magnitude was heterogeneous.DALYs averted/ 10,000 children in Africa ranged from 20.2 (Egypt) to 81.8 (Burkina Faso), median 49.8; in Asia/Pacific/the Middle East from 22.7 (China) to 110.1 (Yemen), median 33.4, and in Latin America from 14.1 (Ecuador) to 68.5 (Bolivia), median 26.5.The median benefit from iron supplements in Africa was 76.4 DALYs averted/10,000 children and ranged from 39.7 in Zimbabwe to 111.6 in Burkina Faso; in Asia/Pacific/Middle East the median benefit was 71.7, ranging from 36.9 in the Phillipines to 133.3 in Pakistan and 133.0 in Yemen; and in Latin America the median benefit was 59.1, ranging from 93.5 in Bolivia to 39.5 in Guatemala. The magnitude of net benefit from MNPs and iron supplements on DALYs was strongly positively associated with the prevalence of moderate anemia (e.g. for MNPs: r=0.82, P=2.3x10-20). In Africa, MNPs cost between $961-$4341/DALY averted; in Asia/Middle-East/Pacific between $844-$3975/DALY averted, and in Latin America between $1306-$6566/DALY averted. The 10 countries where MNPs are most cost-effective were Yemen ($844/DALY averted), Burkina Faso ($961), Mauritania ($1119), The Gambia ($1165), Guinea-Bissau ($1165), Senegal ($1193), Mali ($1197), Guinea ($1267), and Ghana ($1273). Suboptimal coverage markedly reduced both DALYs averted and cost-effectiveness. The severity, not just overall prevalence of anemia, should be considered when planning a programme. Optimisation of programme coverage is essential to maximise cost-effectiveness. Our results augment existing guidelines and identify locations where iron interventions have the greatest benefit and are most cost-effective.
Figure Legend
Caterpillar plots and regional maps demonstrating DALYs averted/ 10,000 children for A) Multiple Micronutrient Powders, and b) Iron Supplements.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal