Abstract
Background: The standard chemotherapy for diffuse large B-cell lymphoma (DLBCL) is CHOP combined with rituximab (R-CHOP). The guidelines (e.g. NCCN or ESMO) recommend six to eight courses of R-CHOP and the optimal number of courses is still unclear. The relative dose intensity (RDI) was proposed as an indicator for both dose intensity and interval. The previous studies have reported the relation between RDI of CHOP or R-CHOP and treatment outcomes. However, little is known about the low threshold of RDI that affects survival and few studies have compared between RDI and total dose of R-CHOP in the effect on survival. In this study, we evaluated the effect of total dose and RDI of R-CHOP on survival in patients with DLBCL.
Patients and methods: We retrospectively analyzed 190 patients with newly diagnosed DLBCL who completed more than 6 courses of R-CHOP between January 2013 and December 2016 at our center. Dose reduction of the CHOP regimen was considered in patients over 70 years of age. RDI was calculated as the ratio of delivered dose intensity (mg/m2/week) to the planned dose intensity (mg/m2/week) and was shown as a percentage. The average of RDI in each drug of R-CHOP was used for the analyses. Risk factors for overall mortality were analyzed using Cox proportional hazards models.
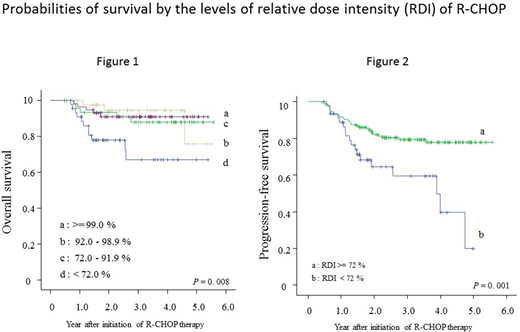
Results: Among the 190 patients, median age was 70.0 years (range, 34-91). The numbers of patients were 15, 55, 46, and 66 in low, low-intermediate, high-intermediate, and high risk groups based on the International Prognostic Index (IPI), respectively. Three-year overall survival (OS) was 88%, 100%, and 83% in the patients with 6 (N=64), 7 (N=3), and 8 (N=123) courses of R-CHOP, respectively (p = 0.55). Median RDI was 92% (range, 32 to 117) and the lower quartile of RDI was 72%. Probabilities of OS by the quartile of RDI were shown in Figure 1 and OS was significantly worse in the patients with <72% of RDI than those with ≥72% of RDI (3-year OS, 66% vs 90%; p = 0.001). Subgroup analysis by age (<70 or ≥70 years) showed the similar trend toward worse survival in patients with <72% of RDI in both age groups (<70 years, p=0.001; ≥70 years, p = 0.054). In multivariable analysis, RDI less than 72% (HR, 2.94; 95% CI, 1.25-6.90, p = 0.014) was a significantly important risk factor for mortality, while IPI (HR, 3.2; 95% CI, 0.9-11.4, p = 0.07) or the number of courses of R-CHOP (HR, 1.66; 95% CI, 0.59-4.64, p = 0.34) was not. When analyzing RDI as a continuous variable, RDI (HR, 1.03; 95% CI, 1.01-1.05, p = 0.009) and IPI (HR, 1.49; 95% CI, 1.05-2.12, p = 0.027) were identified as significant risk factors for mortality. Similarly, patients with <72% of RDI had significantly worse progression-free survival (PFS) than those with ≥72% of RDI (Figure 2, 3-year PFS, 59% vs 80%; p = 0.001). However, RDI was not a significantly important risk factor for PFS after adjusting for several factors. Among 190 patients in our cohort, 24 patients died and 17 patients died from recurrence of DLBCL. There is no difference in the number of recurrence between the patients with <72% (N=6) and ≥72% (N=11) of RDI (p = 0.18).
Conclusions: Higher RDI of R-CHOP was significantly associated with a higher survival rate in patients with DLBCL, although it did not reach statistical significance in patients over 70 years of age. More than 72% of RDI should be maintained to obtain better OS and PFS. Increase of total dose of R-CHOP was not related to better survival, resulting from the analysis using the number of treatment courses. We conclude that 6 courses of R-CHOP therapy with higher RDI would be recommended for all ages. Further studies are needed to validate our findings.
Minami:Novartis Pharma K.K.: Consultancy; Takeda Pharmaceutical Company Limited.: Consultancy; ONO PHARMACEUTICAL CO., LTD: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal