TO THE EDITOR:
Intravascular large B-cell lymphoma (IVLBCL) is a rare type of extranodal diffuse large B-cell lymphoma (DLBCL) characterized by proliferation of neoplastic cells within the vascular lumen, especially within capillaries.1 Diagnosis of IVLBCL is often challenging because of the absence of lymphadenopathy and the variety of symptoms. Nonetheless, diagnosis using random skin biopsy (RSB) from normal-appearing skin has allowed early diagnoses to be possible for many patients.2-4 Because of the rarity of IVLBCL and the uncertainty of its diagnosis, especially in cases with negative biopsy results, the sensitivity and specificity of RSB-based diagnosis have yet to be studied. Here, we have provided an updated report of our experiences with RSBs. Additionally, we have retrospectively analyzed the final diagnosis of consecutive patients who received RSBs at our hospital because IVLBCL was suspected.
We retrospectively reviewed consecutive patients who received RSBs for suspected IVLBCL from June 2006 to August 2018 at Kameda Medical Center (Kamogawa-shi, Japan). Dermatologists were requested to perform incisional RSBs if patients were suspected of having IVLBCL. The biopsied specimens were usually obtained from 3 separate, fat-containing areas of the skin, including the thigh, abdomen, and upper arm. These areas were chosen because intravascular lesions of IVLBCL usually present in capillaries of subcutaneous adipose tissues (supplemental Figure 1, available on the Blood Web site).2,4 Written informed consent for RSB was obtained from each patient or his or her family. The study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review board of Kameda Medical Center.
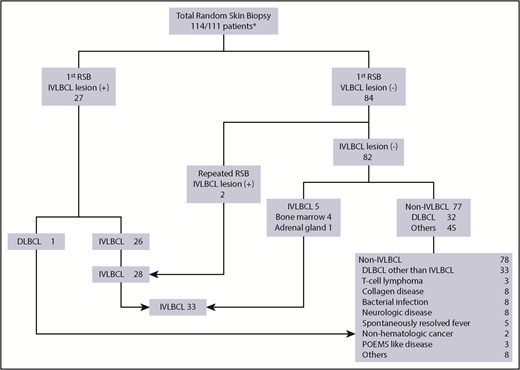
A total of 111 patients received 114 RSBs. Patients were referred to dermatologists by clinicians in the following specialties: hematology/oncology (n = 77), rheumatology (n = 9), general internal medicine (n = 11), neurology (n = 11), and others (n = 3). Figure 1 shows a flow diagram illustrating the of diagnosis of IVLBCL by RSB. Based on the diagnostic workup, the patients were diagnosed with IVLBCL (n = 33); DLBCL other than IVLBCL (n = 33); peripheral T-cell lymphoma (n = 3); collagen disease (n = 8), neurologic disease (n = 8); bacterial infection (n = 8); spontaneously resolved fever (n = 5); nonhematologic cancer (n = 2); polyneuropathy, organomegaly, endocrinopathy, monoclonal paraprotein, and skin changes syndrome (n = 3); and others (n = 8). IVLBCL lesions were detected in 27 patients on first RSBs (24.3%); the remaining 84 patients were negative for IVLBCL lesions. Among the 27 patients who were positive for IVLBCL lesion, 1 was not diagnosed with IVLBCL according to the World Health Organization criteria1 because the patient had a concurrent large cardiac DLBCL and 18F-fluorodeoxyglucose-avid adrenal tumor on positron emission tomography.5 Among the 84 patients who were negative for IVLBCL lesion on their first RSB, 2 were ultimately diagnosed with IVLBCL through a later RSB (a second RSB and a third RSB, specifically). Five patients were subsequently diagnosed with IVLBCL through other means (bone marrow biopsy, n = 4; adrenal biopsy, n = 1). Therefore, 78 patients were ultimately not diagnosed with IVLBCL. Thirty-three of these 78 patients (42.3%) were ultimately diagnosed with DLBCL, all of whom had extranodal involvements, such as of the bone marrow (n = 14), adrenal gland (n = 7), central nervous system (n = 5), testis (n = 2), or other sites. Nodal involvement and splenic involvement were seen in 14 and 12 patients, respectively. Although there are several different diagnostic definitions, 12 of these patients were considered to have primary bone marrow or splenic DLBCL that was devoid of prominent nodal lymphadenopathy (<2 cm in diameter).6-8
Flow diagram depicting the diagnosis of IVLBCL using RSB. Among the 111 patients, 27 had IVLBCL lesion detected on the first RSB; the remaining 84 did not have any IVLBCL lesions. Two patients with negative first RSB findings subsequently had IVLBCL lesions detected on their second and third RSBs. Among the 82 remaining patients with negative RSB, 5 were diagnosed with IVLBCL lesions using bone marrow biopsy (n = 4) and adrenal biopsy (n = 1). One patient with positive RSB findings had concomitant large cardiac B-cell lymphoma and adrenal swelling and therefore was not considered have IVLBCL based on the World Health Organization definition of IVLBCL. In total, 33 patients were diagnosed with IVLBCL; the remaining 78 patients tested negative for IVLBCL. POEMS, polyneuropathy, organomegaly, endocrinopathy, monoclonal paraprotein, skin changes syndrome.
Flow diagram depicting the diagnosis of IVLBCL using RSB. Among the 111 patients, 27 had IVLBCL lesion detected on the first RSB; the remaining 84 did not have any IVLBCL lesions. Two patients with negative first RSB findings subsequently had IVLBCL lesions detected on their second and third RSBs. Among the 82 remaining patients with negative RSB, 5 were diagnosed with IVLBCL lesions using bone marrow biopsy (n = 4) and adrenal biopsy (n = 1). One patient with positive RSB findings had concomitant large cardiac B-cell lymphoma and adrenal swelling and therefore was not considered have IVLBCL based on the World Health Organization definition of IVLBCL. In total, 33 patients were diagnosed with IVLBCL; the remaining 78 patients tested negative for IVLBCL. POEMS, polyneuropathy, organomegaly, endocrinopathy, monoclonal paraprotein, skin changes syndrome.
Based on the results reported here, it was calculated that RSB had a 77.8% sensitivity and 98.7% specificity for diagnosis of IVLBCL. The positive and negative predictive values of RSB were 96.6% and 90.6%, respectively.
When clinical characteristics related to the positivity and negativity of RSB were compared, the patients with positive RSB findings were significantly more likely to have unexplained fever, alteration of consciousness, and hypoxemia. Further, the group of patients with positive RSB findings had significantly lower platelet counts, significantly higher lactate dehydrogenase (LDH), and significantly higher soluble interleukin-2 receptor (sIL2R) levels. Serum ferritin levels did not significantly differ between the 2 groups (supplemental Table 1). Among the 28 patients who were positive for RSB and diagnosed as with IVLBCL, bone marrow involvement was detected in 18 (64.3%), whereas among the 5 patients who were diagnosed with IVLBCL other than RSB, 4 (80.0%) were positive for bone marrow involvement.
Next, we evaluated predictors for RSB positivity. Using receiver operating characteristic curve analyses to select cutoff values (supplemental Figure 2), the following variables were associated with RSB positivity: unexplained fever ≥38°C, alteration of consciousness, O2 saturation ≤95%, platelet count <120 × 109/L, serum LDH value >800 U/L, and serum sIL2R level >5000 U/mL. For each of these factors that was present, we assigned patients a score of 1. The percentages of patients with scores of 0, 1, 2, 3, 4, 5, and 6 who had positive RSB findings were 0% (0/13), 0% (0/23), 0% (0/13), 30% (6/20), 36.4% (8/22), 45.5% (5/11), and 83.3% (10/12), respectively. Among the 49 patients with scores of 0 to 2, none had positive results on RSB. However, among the 23 patients with scores of 5 to 6, 15 (65.2%) had positive results. Patients with scores of 3 to 4 had intermediate positivity (14/42. 33.3%) (Table 1). These results should help to determine the indication of RSB for patients suspected of having IVLBCL.
Proportions of patients with or without IVLBCL lesions, based on the number of predicting factors
| No. of predictive factors . | IVLBCL lesion (+), n = 29 . | IVLBCL lesion (−), n = 86 . | RSB, % positive . |
|---|---|---|---|
| 0-2 | 0 | 49 | 0 |
| 3-4 | 14 | 28 | 33.3 |
| 5-6 | 15 | 8 | 65.2 |
| No. of predictive factors . | IVLBCL lesion (+), n = 29 . | IVLBCL lesion (−), n = 86 . | RSB, % positive . |
|---|---|---|---|
| 0-2 | 0 | 49 | 0 |
| 3-4 | 14 | 28 | 33.3 |
| 5-6 | 15 | 8 | 65.2 |
Predictive factors: unexplained fever, ≥38°C; alteration of consciousness; O2 saturation, ≤95%; platelet count, <120 × 109/L; serum LDH level, >800 U/L; and serum sIL2R level, >5000 U/mL.
The high RSB sensitivity in the present study contrasts with a recent report from the United States, in which RSBs appeared to have limited capability for diagnosis IVLBCL.9 In a recent report from Canada,10 IVLBC was diagnosed using skin lesions in 38% of patients. The sensitivity of RSB is thought to depend on the skin biopsy method used. We noted that most of the histologic images of IVLBCL reported from the United States and European countries used punch biopsies with 4 to 5 mm of depth, which thus did not contain sufficient adipose tissue. Most patients who have IVLBCL lesions in the dermis also have IVLBCL lesions in deep adipose tissue,2,4 but the opposite statement is not true. No clear difference was noted on the positivity of IVLBCL lesion according to the topographic sites.
The cutaneous variant of IVLBCL,11 which is exclusively diagnosed in Western IVLBCL patients, was not observed in our series. We recently reported that approximately one-half of the patients had IVLBCL lesions in deep adipose tissues only12 that do not develop skin changes. However, the presence or absence of IVLBCL lesions in the hypodermic adipose tissues of normal-appearing skin have not been mentioned in reports of Western patients with cutaneous-variant IVLBCL.
There are several limitations to this study. In addition to the retrospective nature of the study, RSB was not performed according to the predetermined criteria because the physicians in various specialties at our hospital referred patients requiring RSB to the dermatology department. However, this study is the first to longitudinally evaluate the sensitivity and specificity of RSBs in a relatively large cohort. We also provided information on the important determinant factors that could indicate the need for RSBs in patients who are suspected of having IVLBCL.
We conclude that the good performance of RSBs for patients suspected of having IVLBCL could provide earlier diagnosis and, in turn, could improve prognoses.
The online version of this article contains a data supplement.
Acknowledgments
The authors thank all of the technicians of the Clinical Pathology Department at the Kameda Medical Center, especially Kaori Kumata for her excellent technical assistance on this study. The authors also thank the many residents at the Department of Hematology/Oncology of Kameda Medical Center who provided medical care to the patients during the study period. They also thank Editage (www.editage.jp) for English language editing.
Authorship
Contribution: K.M. conceived and designed the study and wrote the manuscript; K.M. and N.E. collected the data; Y.A. performed the statistical analysis; K.M., Y.A., A.K., K.N., D.M., H.K., and M.T. provided medical care of the patients; N.E. and A.T. performed the random skin biopsies; K.T. reviewed the pathologic specimens and made the diagnoses; and all authors reviewed and approved the final manuscript.
Conflict-of-interest disclosure: K.M. received honoraria from Celgene Corporation. The remaining authors declare no competing financial interests.
Correspondence: Kosei Matsue, Division of Hematology/Oncology, Department of Medicine, Kameda Medical Center, 929 Higashi-chou, Kamogawa-shi, Chiba 296-8602, Japan; e-mail: koseimatsue@gmail.com.