BACKGROUND: In sickle cell disease (SCD), preventing all pain crises or other serious complications is not possible. When consistently followed by a health provider, some complications are avoidable. Patients lose vital opportunities for health monitoring/education when appointments are missed, increasing risk of hospitalization or mortality. Forgetfulness, disease risk/symptom severity perception, transportation, long clinic wait times, scheduling and work/school commitments are examples of factors keeping patients from appointments. An understanding of relevant benefits of and barriers to appointment keeping is essential to overcoming the barriers and promoting the benefits. Appointment keeping behaviors are multi-dimensional and often related to many of the social determinants of health. The Health Belief Model (HBM) is a theoretical framework previously used to investigate appointment keeping. Exploring an individual's general health motivations, perceived disease risks and the role of specific behaviors to reduce risks can be informative in this context.
OBJECTIVE: The purpose of this research was to explore how health beliefs affect the appointment keeping behavior of pediatric SCD patients and caregivers at a hospital-based outpatient clinic in central Illinois.
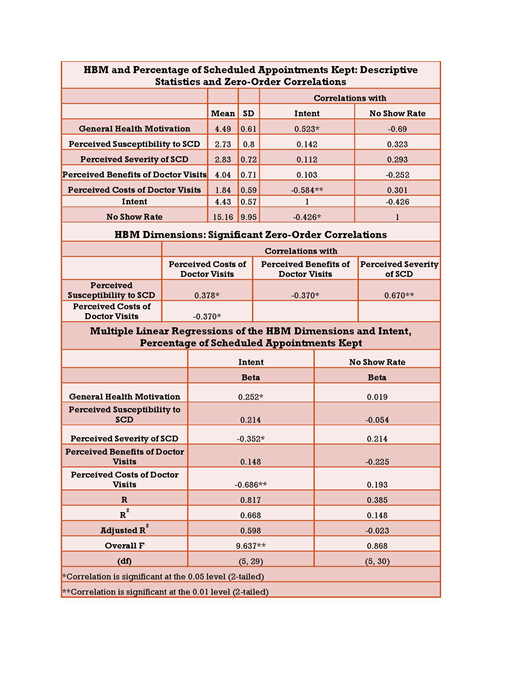
METHODS: A 53 question multiple-choice questionnaire was utilized to assess health beliefs. This modified version of a validated HBM questionnaire was changed with permission from the creator (Mirotznik et al., 1998) to better represent the symptoms/complications of SCD. Questions determined participants' general health motivation (GHM), perceived susceptibility to the complications of SCD (PSC), perceived severity of SCD (PS), perceived benefits of doctor visits (PB), perceived costs of doctor visits (PC) (i.e. finding transportation, the energy or time to keep visit, wait at clinic, having blood drawn, talking multiple people at one visit, etc.) and intent to keep doctor appointments (INT). The Cronbach alpha coefficient was .87, suggesting good internal consistency reliability. Participants were recruited through convenience sampling at scheduled clinic appointments. A chart review measured overall appointment keeping.
RESULTS: In total, 32 individuals (caregiver or patient ≥14 years) completed the questionnaire. There was a significant difference in 'no show' appointment rates for males versus females (Mean= 5.4% 'no show' rate for males vs Mean=17.6% for females, p=.008, two-tailed t-test). There was not a significant difference in 'no show' rates based on the gender of the child (<14 years), participant's city of residence or child's SCD type. There was a small, positive correlation between the age of the child and 'no show' rate (r =.175), but it was not statistically significant. There were statistically significant correlations between INT and GHM (r =.523), PC (r = -.584), and 'no show' rates (r = -.426). PSC had statistically significant correlations with PS (r =.670), PB (r = -.370), and PC (r = .378). PB had a statistically significant correlation with PC (r = -.370). A regression analysis for INT with GHM, PSC, PS, PB and PC as variables explained 66.8% of the variance in intent. Of all the variables, PC made the largest unique contribution (beta = -.69). PS and GHM also made statistically significant contributions (beta = -.35 and .25, respectively).
CONCLUSIONS: Three HBM dimensions were uniquely associated with INT. GHM was positively associated, PS negatively associated and PC negatively associated. Participants' PSC and PS play an important role in the perception of the benefits and costs to appointment attendance. Future work to improve appointment keeping will require a larger focus on minimizing costs of doctor visits. Furthermore, effectively enhancing GHM could also improve attendance, potentially lessening the disease process and improving overall wellness. PS negatively correlates with INT. Although counterintuitive, these findings are congruent with those found in lupus patients by Mirotznik et al. Patients with higher PS may have acute medical visits more often, leaving them unable to attend additional scheduled preventative visits because of the costs. Additionally, if some preventative care tasks are added to acute visits when appropriate (as in our institution), the patients/caregivers may see less benefit in attending the next scheduled comprehensive visit.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal