Introduction
Incidence of hospital-acquired venous thromboembolism (HA-VTE) in children has been increasing in the absence of proven effective preventative interventions. To decrease the incidence of HA-VTE, we must first identify children at the highest risk by creating a risk assessment model (RAM). Critically ill children, especially those with a central venous catheter (CVC), inflammatory condition and/or prolonged hospital stay have been identified as high-risk. To date, studies of HA-VTE in critically ill children have only been at single-center and have not been well-validated in diverse populations. The Children's Hospital-Acquired Thrombosis (CHAT) consortium established a large multicenter Registry to develop and validate pediatric RAMs for HA-VTE. This multicenter study aimed to derive a RAM for HA-VTE among critically ill children (RAM-ICU) performed upon admission/transfer to a pediatric intensive care unit (PICU).
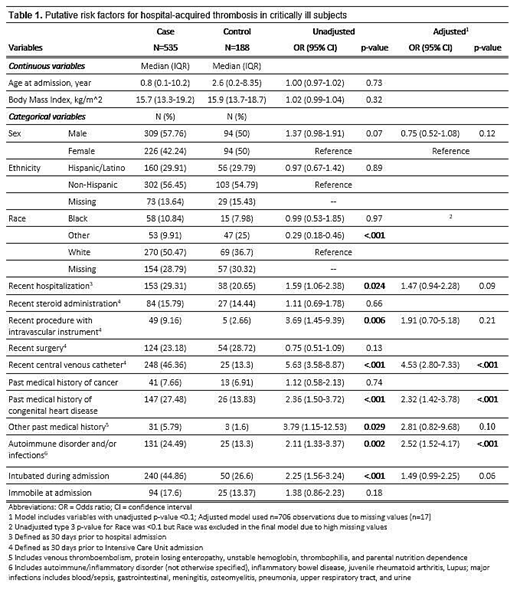
The CHAT Registry consists of retrospectively-identified, imaging confirmed cases of symptomatic HA-VTE and hospitalized controls (without HA-VTE) aged 0-21 years from eight U.S. centers. Controls were frequency-matched by year of admission and center. Details on demographics, medical history and hospital course were extracted from the medical record. For the RAM-ICU, only HA-VTE subjects and controls admitted/transferred into an ICU were included. Subjects who had a cardiac surgery up to 2 weeks prior to ICU admission were excluded. Fourteen variables that were present at or within 24 hours of ICU admission/transfer were evaluated by univariate logistic regression. These included demographics, medications, medical history, recent surgeries, mechanical ventilation, patient mobility and presence of a CVC. Those variables with p-values of <0.1 in univariate analyses were included in a multivariable logistic regression model. For the final model, variables with p-values of <0.05 were considered statistically significant.
Results
Out of 1172 HA-VTE cases and 952 controls in the Registry, 535 cases and 188 controls met inclusion criteria for the RAM-ICU. With discrepant subject distribution as expected due to previously reported increased incidence of HA-VTE in critically ill children. Median age was 0.8 years (IQR 0.1-10.2) for cases and 2.6 years (IQR 0.2-8.35) for controls. Fifty-eight percent of cases and 50% of controls were male. The Table presents the unadjusted analysis which revealed eight variables associated with HA-VTE (P<0.05): recent hospitalization (prior to current hospitalization), procedure with intravascular instruments within 24 hours of ICU admission, CVC present or placed within 24 hours of ICU admission, congenital heart disease, autoimmune disease or serious infection (includes autoimmune/inflammatory disorder, inflammatory bowel disease, juvenile rheumatoid arthritis, lupus, or major blood, organ or urinary infection), mechanical ventilation within 24 hours of ICU admission, and other past medical history (Table). Variables that remained statistically-significant, independent risk factors in an adjusted (multivariable) logistic regression included presence of a CVC (4.53; 95% CI=2.80-7.33), congenital heart disease (OR=2.32; 95% CI=1.42-3.78), and autoimmune disease or serious infection (OR=2.52; 95% CI=1.52-4.17) (Table).
Conclusions
With the increasing incidence of pediatric HA-VTE, there is an urgent need to identify children at high risk and incorporate risk reduction methods. The CHAT RAM-ICU represents the largest, multicenter pediatric study evaluating HA-VTE risk in children admitted/transferred to an ICU, with 535 HA-VTE cases and 188 controls. Recent placement of a CVC, congenital heart disease, and autoimmune disease or serious infection are significant, independent risk factors for HA-VTE in critically ill children. We will prospectively validate the RAM-ICU in a multicenter prospective study funded via the Hemophilia and Thrombosis Research Society.
Jaffray:CSL Behring: Research Funding. Mahajerin:Alexion: Speakers Bureau; Genentech: Consultancy, Speakers Bureau; Kedrion: Membership on an entity's Board of Directors or advisory committees; Spark: Speakers Bureau. Silvey:Genentech: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Bayer: Membership on an entity's Board of Directors or advisory committees. Croteau:Spark Therapeutics: Research Funding; Spark Therapeutics: Research Funding; Novo Nordisk: Consultancy, Honoraria, Research Funding; Novo Nordisk: Consultancy, Honoraria, Research Funding; Shire: Consultancy, Honoraria; Shire: Consultancy, Honoraria; CSL Behring: Consultancy, Honoraria; CSL Behring: Consultancy, Honoraria; Bayer: Consultancy, Honoraria; Bayer: Consultancy, Honoraria; Pfizer: Research Funding; Genentech: Consultancy, Honoraria; Pfizer: Research Funding; Octapharma: Honoraria; Genentech: Consultancy, Honoraria; Octapharma: Honoraria. Young:CSL Behring: Consultancy, Honoraria; Bioverativ/Sanofi: Consultancy, Honoraria; Freeline: Consultancy, Honoraria; Genentech/Roche: Consultancy, Honoraria, Research Funding; Grifols: Consultancy, Honoraria; Kedrion: Consultancy, Honoraria; Novo Nordisk: Consultancy, Honoraria; Spark: Consultancy, Honoraria; Shire/Takeda: Consultancy, Honoraria; Uniqure: Consultancy, Honoraria. Goldenberg:NIH: Other: research support and salary support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal