Background: Since FLT3-ITD is a poor prognostic factor for acute myeloid leukemia (AML), allogeneic hematopoietic stem cell transplantation (allo-HSCT) is practically performed. However, clinical usefulness of allo-HSCT at the first remission (CR1) has not been fully evaluated by the prospective study. To prospectively elucidate the role of allo-HSCT at CR1 in younger adult patients with FLT3-ITD positive AML and explore the prognostic impacts of clinical and genetic features, we conducted a phase II multicenter study (JALSG AML209-FLT3-SCT, UMIN Clinical Trials Registry UMIN000003433, http://www.umin.ac.jp/ctr/).
Methods: A total of 49 patients 16 to 49 years of age with newly diagnosed de novo AML were enrolled in this study if they had a FLT3-ITD mutation and achieved complete remission within 2 courses of the standard induction therapies consisting of cytarabine and either daunorubicin or idarubicin. All patients were to be received allo-HSCT as soon as possible while continuing 4 courses of consolidation therapy combining cytarabine plus mitoxantrone, daunorubicin, aclarubicin or etoposide, vincristine, and vindesine. Patients received no further chemotherapy until allo-HSCT or relapse. Conditioning was selected according to each institutional standard from myeloablative regimens except for reduced intensity conditioning only in patients older than 40 years old or with higher HCT-CI than 1 point. GvHD prophylaxis was according to each institutional standard based on cyclosporine A or tacrolimus combined with short-term MTX.
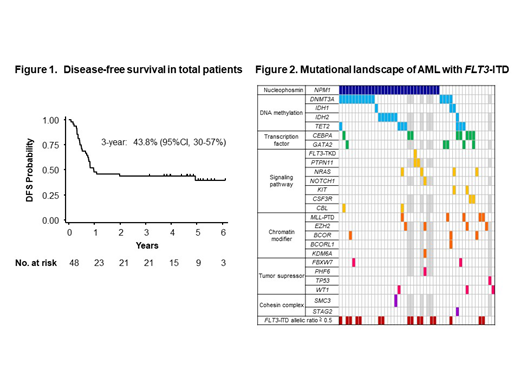
Targeted sequencing of 57 genes frequently identified in myeloid malignancies were analyzed using the preserved DNA extracted from AML cells at diagnosis. FLT3-ITD allelic ratio (AR) was quantified using DNA fragment analysis. Primary endpoint was 3-year disease-free survival (DFS).
Results: Among 48 eligible patients with the median age of 38.5 (range, 17-49) years, 36 (75%) maintained CR1 to receive allo-HSCT at the median of 108 (range, 54-228) days after the achievement of CR1. Median follow-up was 1,726 (range, 983-2,974) days. The 3-year DFS rate was 43.8% (95% confidence interval [CI], 30-57%, Figure 1). The lower limit of 95% CI exceeded threshold response rate of 20%, concluding the treatment was effective. The 3-year overall survival, post-transplant DFS and non-relapse mortality rates were 54.2% (95%CI, 39-67%), 58.3 % (95%CI, 41-72%) and 25.0% (95%CI, 12-40%), respectively. There was no significant difference in DFS post allo-HSCT according to donor sources (related BM 64.6% vs. related PB 50.0% vs. unrelated BM 63.6% vs. UCB 60.0% at 3 years, P= .881). Neutrophil recovery was achieved in 94.3%. Cumulative incidences of grade II to IV and III to IV acute GvHD at day 100 were 21.2% (95%CI, 9-37%) and 9.1% (95%CI, 2-22%), respectively. Cumulative incidence of chronic GvHD at 1 year was 25.0% (95%CI, 12-40%).
Mutations in NPM1 gene (65%) and genes associated with DNA methylation were frequently identified including DNMT3A (36%), IDH1 (6%), IDH2 (17%) and TET2 (17%, Figure 2). Median ITD AR was 0.344 (range, 0.006-4.099). There was no significant overlap of genetic alterations with high ITD-AR (≥ 0.5). No significant impact on DFS was observed by high ITD AR (≥0.5) (Hazard ratio [HR], 1.53; 95%CI, 0.58-4.06; P= .39) or other co-occurring genetic alterations including NPM1 mutations (HR, 0.78; 95%CI, 0.28-2.20; P= .64).
Conclusions: This prospective study demonstrated the efficacy and safety of proceeding faster to allo-HSCT in CR1 for younger adult patients with FLT3-ITD positive AML, whose graft sources were not limited to HLA identical donors and the first available donor should be considered. Beyond FLT3-ITD mutations, no significant prognostic factor was identified in their genetic background or high ITD AR. Further study is required to improve the prognosis of AML patients with FLT3-ITD by establishment of an adequate therapeutic strategy using FLT3 inhibitors and allo-HSCT.
Atsuta:Kyowa Kirin Co., Ltd: Honoraria; Mochida Pharmaceutical Co. Ltd: Honoraria; Chugai Pharmaceutical Co., Ltd.: Honoraria; Janssen Paharmaceutical K.K.: Honoraria. Sawa:Asahi-Kasei: Honoraria; Celgene: Honoraria; Sumitomo Dainippon Pharma: Honoraria; MSD: Honoraria; Mochida: Honoraria; Ono Pharmaceutical Co., Ltd: Honoraria; Bristol-Myers Squibb: Honoraria; Takeda: Honoraria; Sanofi: Honoraria; Chugai Pharmaceutical Co., Ltd.: Honoraria; Astellas Pharma Inc.: Honoraria; Kyowa-Hakko Kirin: Honoraria; Nippon Shinyaku: Honoraria; Pfizer Japan Inc.: Honoraria; Novartis: Honoraria; Eisai: Honoraria; Otsuka Pharmaceutical: Honoraria; Shire: Honoraria; Mundi Pharma: Honoraria. Ozawa:Kyowa-Hakko Kirin: Honoraria; Novartis: Honoraria; Pfizer Japan Inc.: Honoraria; Astellas Pharma Inc.: Honoraria. Tomita:Taiho Pharma: Research Funding; Kyowa Kirin: Research Funding; Chugai Pharmaceutical Co., Ltd.: Honoraria, Research Funding. Maeda:Nippon Shinyaku Co., Ltd.: Honoraria; Janssen Pharmaceutical K.K..: Honoraria. Usuki:Daiichi Sankyo Co., Ltd.: Research Funding, Speakers Bureau; Astellas Pharma Inc: Research Funding, Speakers Bureau. Matsuoka:Takeda Pharmaceutical: Research Funding; Novartis: Research Funding; Astellas Amgen Biopharma: Consultancy. Asou:SRL Inc.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding; Astellas Pharm Inc.: Research Funding; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding; Asahi Kasei Pharma Co., Ltd.: Research Funding; Eisai Co., Ltd: Research Funding; Novartis Pharmaceuticals: Research Funding; Nippon Shinyaku Co., Ltd.: Research Funding; Kyowa Hakko Kirin Co., Ltd.: Research Funding. Matsumura:Otsuka Pharmaceutical: Consultancy, Research Funding; Novartis: Speakers Bureau; Bristol-Myers Squibb: Speakers Bureau; Pfizer: Research Funding, Speakers Bureau. Miyazaki:Kyowa-Kirin: Honoraria; Dainippon-Sumitomo: Honoraria; Chugai: Research Funding; Nippon-Shinyaku: Honoraria; Novartis: Honoraria; Otsuka: Honoraria. Kiyoi:Otsuka Pharmaceutical Co.,Ltd.: Research Funding; Astellas Pharma Inc.: Honoraria, Research Funding; Pfizer Japan Inc.: Honoraria; Zenyaku Kogyo Co., Ltd.: Research Funding; Eisai Co., Ltd.: Research Funding; Bristol-Myers Squibb: Research Funding; Kyowa Hakko Kirin Co., Ltd.: Research Funding; Perseus Proteomics Inc.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding; Daiichi Sankyo Co., Ltd: Research Funding; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding; Takeda Pharmaceutical Co., Ltd.: Research Funding; Nippon Shinyaku Co., Ltd.: Research Funding; FUJIFILM Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal