
Purpose
Vincristine (VCR) is frequently used for the treatment of pediatric cancer. However, it can lead to dose-limiting vincristine-induced peripheral neuropathy (VIPN). This study aimed to investigate if prolonging the duration of VCR administration (1-hour infusions instead of push injections) reduces VIPN in children with cancer during the first year of treatment.
Methods
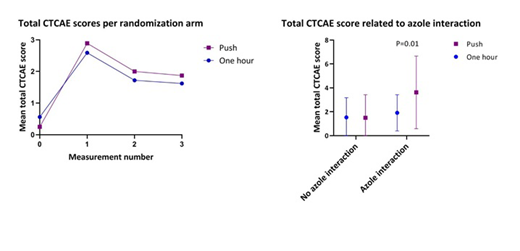
The VINCA trial is an international multicenter randomized controlled trial. Participants were randomized to receive all VCR administrations through push injections or 1-hour infusions. Dose of VCR was 1.5-2 mg/m2 with a maximum of 2 mg. VIPN measurements were performed at baseline and 1-3 times during treatment, depending on the number of VCR administrations and the total treatment time, using 4 items of the common toxicity criteria of adverse events (CTCAE version 4.03): constipation, peripheral sensory neuropathy, peripheral motor neuropathy and neuralgia. Individual item scores range from zero (no complaints) to five (death). The primary outcome of this trial was total sum CTCAE score during first year of treatment. For the current analysis, patients treated for acute lymphoblastic leukemia (ALL) or Hodgkin's lymphoma were included. All included patients were analyzed according to the intention-to-treat principle. Besides VIPN measurements, data on all relevant co-medication during treatment were collected, including data of concurrent azole therapy (as azole treatment is known to interact with VCR treatment). Descriptive data were analyzed using either chi-square tests or t-tests. Longitudinal data were analyzed using repeated measures mixed model analysis for continuous outcomes (total CTCAE sum score) and generalized estimating equations for dichotomous outcomes (having VIPN yes or no, with VIPN defined as a CTCAE score of ≥ 2 on any of the 4 CTCAE items). Patients were considered to have been treated with concurrent azole therapy when azoles were used during the week before or following VCR administration and if ≥ 50% of VCR administrations between two succeeding measurements were given with concurrent azole therapy. Results were corrected for concurrent azole therapy, cumulative VCR dose, disease, age, gender, ethnicity and time since diagnosis.
Results
In total 90 children (n=45 one hour infusions group, n=45 push injections group) participated in the study, 58 (64%) with ALL and 18 (20%) with HL. Participants in the two randomization groups did not significantly differ regarding gender, age, ethnicity, diagnosis, or cumulative VCR dose. Overall results showed no effect of randomization on total CTCAE score (β=0.07, 95% confidence interval (CI) -0.42-0.56, p=0.78). However, concurrent azole treatment appeared to be an effect modifier in this analysis and therefore results are reported separately for measurements with (n=24) and without concurrent azole therapy (n=226). Among patients who received concurrent azole therapy, total CTCAE sum score was significantly higher in the push group compared to the 1-hour group (β=1.95, 95% CI 0.49-3.41, p=0.01), while among those without concurrent azole therapy, these CTCAE sum scores did not differ between the two randomization groups (β=-0.17, 95% CI: -0.67-0.34, p=0.52). The risk of developing VIPN (no/yes) did not significantly differ between both randomization groups, irrespective whether concurrent azole treatment was given or not (with azole: OR (95% CI)=4.92 (0.60-40.37), p=0.14; without azole: OR (95% CI)=0.97 (0.51-1.82, p=0.92).
Conclusions
Overall, administration method of VCR given as push injection or 1-hour infusion did not seem to affect the risk of developing VIPN in children treated for ALL or HL when using the current dosing regimen. However, when concurrent azole treatment is given, total CTCAE scores are significantly lower in children in the 1-hour infusion group compared to the push injection group, demonstrating less VIPN. These results indicate that for children treated with VCR and concurrent azole therapy for the prevention or treatment of fungal infections, administration of VCR by 1-hour infusions instead of push injections is recommended.
Kaspers:Helsinn Healthcare: Consultancy; Boehringer Ingelheim Pharma: Other: Member of a DSMC. van der Sluis:medac: Consultancy; jazz farmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal