Introduction: Primary Mediastinal B-cell Lymphoma (PMBCL) is a rare, aggressive disorder that predominantly afflicts younger women and accounts for approximately 2% of all Non-Hodgkin-lymphoma. Due to the rarity of PMBCL and thus lack of prospective trials performed, there is no established standard of care. In the pre-rituximab era more intensive regimens resulted in superior outcomes compared to the CHOP-regimen, a difference that appears to be abrogated by the addition of rituximab. Also, early trials suggested that radiotherapy (RT) was a critical component of treatment and is commonly incorporated in the treatment strategy. However, the necessity of RT has been debated, due to its potential long-term consequences. Recent trials have evaluated the dose-intensive regimen DA-EPOCH-R with omission of RT, and have showed promising outcomes, albeit so far in non-randomised settings. Further, some retrospective studies have demonstrated encouraging results also with other chemotherapy regimens without RT. Thus, the optimal treatment strategy for adult patients with PMBCL remains undefined. We aimed to describe the PMBCL population diagnosed in Sweden 2007-2017 and to evaluate overall survival by chemotherapy and use of consolidative RT.
Methods: The study population was identified via the Swedish lymphoma register (SLR, >95% national coverage). A central pathology review is ongoing to verify PMBCL diagnosis. Data regarding prognostic factors, treatment and survival among all patients diagnosed with PMBCL 2007-2017 was retrieved. Overall survival (OS) proportions were computed and illustrated using the Kaplan-Meier method. Multivariable Cox regression analysis was used to investigate associations with treatment and outcome by age.
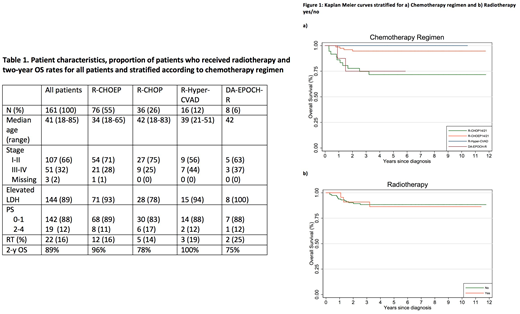
Results: During the time period studied 161 patients were registered with a PMBCL diagnosis in the SLR, of whom 58% were female. Median age was 37 years (range 18-85). Regarding prognostic factors, 66% presented with stage I-II disease, 89% with elevated lactate dehydrogenase (LDH) and 88% with performance status (PS) score of 0-1. Treatment information was available for 137 (85%) patients. The most commonly administered regimen was R-CHOEP-14 (n=76, 55%). Sixteen (12%) received R-Hyper-CVAD, 36 (26%) R-CHOP-14/21, 8 (6%) DA-EPOCH-R and 1 (1%) R-VACOP-B. Median age slightly differed between regimens and was highest among patients administered R-CHOP (42 years) and DA-EPOCH-R (40 years), compared to 34 and 39 years for patients administered R-CHOEP-14/21 and R-Hyper-CVAD, respectively. Apart from age, patient characteristics were similar between regimens (Table 1). Use of consolidative RT was similar for all regimens, and was only applied to 22/137 (16%) of all patients. Patient characteristics for patients with/without RT were similar. Two-year overall survival (OS) rates for all patients was 89% (95% CI:83-93%), 78% (95% CI: 60-88%) with R-CHOP-14/21, 75% (95% CI: 31-93%) with DA-EPOCH-R, 96% (95% CI:88-99%) with R-CHOEP and 100% with R-Hyper-CVAD (Figure 1a). Two-year OS-rates for patients who received RT was 91% (95% CI: 68-98%), compared to 90% (95% CI: 83-94%) for patients who did not received RT (Figure 1b). In a multivariable analysis adjusting for age with R-CHOEP as reference, the hazard ratio for treatment with R-CHOP was 3.6 (95% CI: 0.99-13, p=0.05) and with DA-EPOCH-R 4.6 (95% CI: 0.83-25, p=0.08). As there were only 16 events during the follow-up time, adjustment for further variables was not feasible.
Conclusion: In this population-based study we demonstrate encouraging survival rates for PMBCL patients, of which the majority were managed without RT. In contrast with prior studies that show a promising effect of DA-EPOCH-R for PMBCL patients, patients treated with DA-EPOCH-R in this study had a lower 2-year OS compared to patients treated with the other intensive regimens R-CHOEP and R-Hyper-CVAD. However, the limited number of patients in each treatment group preclude a robust comparison of regimens. Lastly, RT was not associated with a survival benefit in this population-based series.
Smedby:Celgene: Honoraria; Takeda: Research Funding; Janssen Pharmaceuticals: Other: This project was partly funded through a private-public collaboration between KI and Janssen pharmaceuticals..
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal