
Introduction: Severe renal impairment (RI) is a common complication of multiple myeloma (MM). Effective anti-MM therapy and supportive care can restore renal function in several patients, but we lack biomarkers that could predict renal outcomes. Neutrophil gelatinase-associated lipocalin (NGAL) is one of the earliest and most robust markers of acute kidney injury while serum Cystatin C (CysC) reflects renal function more accurately than creatinine and correlates with both tumor burden and renal function in MM. GDF-15 is secreted by bone marrow stromal cells and high serum levels indicate a poor treatment prognosis and a high risk of progression to dialysis in AL amyloidosis. Our aim was to evaluate serum NGAL, CysC, and GDF-15 in MM patients with severe RI defined as eGFR<30 ml/min/1.73m2, by CKD-EPI formula, including those on dialysis, as biomarkers for prediction of renal responses.
Patients & Methods: MM patients who presented with myeloma-related severe RI in the Department of Clinical Therapeutics (Athens, Greece) were included in this study. NGAL, CysC and GDF-15 were measured in the same frozen serum sample collected before the administration of any therapy. Serum NGAL was measured using ELISA (BioPorto Diagnostics A/S, Gentofte, Denmark), while CysC was measured using a latex particle-enhanced nephelometric immunoassay (Dade Behring-Siemens Healthcare Diagnostics, Liederbach, Germany). GDF-15 was measured by a novel immunoassay, the Elecsys GDF-15 assay (Roche Diagnostics International Ltd, Rotkreuz, Switzerland), which is based on the sandwich immunoassay principle using biotin-streptavidin technology. Patients on dialysis received dialysis with regular membranes. IMWG renal response criteria were used.
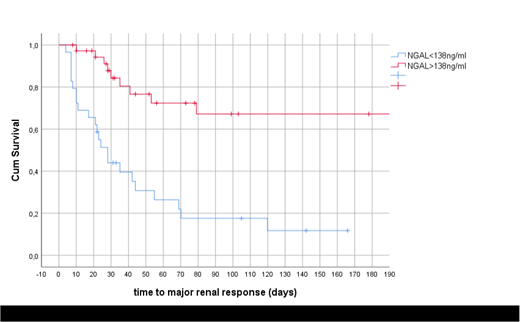
Results: In total, 101 newly diagnosed MM patients with severe RI were included in this analysis. Median creatinine was 4.6 mg/dl (range 2->10 mg/dl), median eGFR (ml/min/1.73 m2) was 11.3 (1.3-29.8) and dialysis was required in 35 (35%) patients. The median age was 71 years; median involved FLC was 4740 mg/L; hypercalcemia was found in 24%, LDH ≥ULN in 44% and high-risk cytogenetics in 25% of patients, while 98% of patients were classified as having ISS-3 and 49% as having R-ISS-3 disease stage. Treatment was bortezomib-based in all patients (in 21% VD and in 79% a triplet: VCD or VTD). Median NGAL levels were 182.3 ng/mL (range 20-550 ng/ml) and of CysC were 3.3 mg/L (0.9-8 mg/L); there was a strong correlation between NGAL and CysC levels (R2=0.653, p<0.001). There was also a strong correlation of both CysC and NGAL with eGFR (for CysC: R2=0.615, p<0.001 and for NGAL: R2=0.464, p<0.001). Both NGAL and CysC levels were higher in patients requiring dialysis vs those not in dialysis (median NGAL: 308 vs 166 ng/mL, p<0.002 and median CysC: 4.99 vs 2.83 mg/L, p=0.008). No significant correlations were observed with GDF-15 and the parameters tested. Renal response (Rrenal) was achieved in 63% of patients, including 45% with major Rrenal. Importantly, 40% of patients who required dialysis became dialysis independent. Median time to Rrenal was one month and median time to dialysis independence was two months. Lower levels of NGAL (p=0.0003) and CysC (p=0.03) were associated with higher probability of major Rrenal among patients with severe RI. Baseline eGFR, levels of sFLC and GDF-15 did not correlate with major Rrenal. None of these markers was associated with probability of dialysis independence among patients who required dialysis. Based on ROC analysis, in patients with severe RI (but not on dialysis), NGAL <138 ng/ml was strongly associated with major Rrenal (80% vs 20% at 3 months, p<0.001; Figure). Regarding CysC, levels <2.9 mg/L were associated with higher probability and shorter time to major Rrenal (p=0.012). In multivariate analysis performed in patients not on dialysis, that included age, NGAL, CysC and eGFR, only NGAL <138ng/ml remained a significant prognostic factor associated with major Rrenal (HR 5, 95% CI 2-18, p=0.002).
Conclusions: Serum levels of NGAL were independent predictors of major renal response in MM patients with severe RI. Thus, serum NGAL could identify MM patients with severe RI who should be treated with more aggressive therapies and more effective and rapidly acting antimyeloma regimens. The absence of any predictive value of GDF-15 in MM-related severe RI in contrast to AL amyloidosis patients reflect the different biology of RI in these plasma cell dyscrasias.
Dimopoulos:Sanofi Oncology: Research Funding. Kastritis:Amgen: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Genesis: Honoraria; Prothena: Honoraria; Pfizer: Honoraria; Takeda: Honoraria. Papassotiriou:Roche: Employment. Gavriatopoulou:Amgen: Honoraria; Janssen: Honoraria, Other: Travel expenses; Genesis: Honoraria, Other: Travel expenses; Takeda: Honoraria, Other: Travel expenses. Terpos:Janssen: Honoraria, Other: Travel expenses, Research Funding; Amgen: Honoraria, Research Funding; Celgene: Honoraria; Takeda: Honoraria, Other: Travel expenses, Research Funding; Genesis: Honoraria, Other: Travel expenses, Research Funding; Medison: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal