Background: Sickle cell disease (SCD) is an inherited hemoglobinopathy which affects over 300,000 children born each year worldwide. In spite of improvement in supportive care in recent years, there is still a lack of effective treatment options. SCD leads to debilitating and cyclic episodes of erythrocyte sickling with progressive organ injury, contributing to lifetime morbidity and shortened life expectancy. Allogeneic HCT (allo-HCT) is a potentially curative therapy for SCD because engraftment is associated with resolution of the clinical phenotype of the disease and abrogation of its complications. Medical literature on allo-HCT for SCD is largely limited to children. Recent studies have evaluated the efficacy of allo-HCT in the adult population. Here, we conduct a systematic review/meta-analysis to assess the totality of evidence pertaining to the efficacy (or lack thereof) of allo-HCT in children and adults.
Materials and methods: We performed a comprehensive search of the medical literature using PubMed/Medline, EMBASE and Cochrane library on July 3rd, 2019. We extracted data on clinical outcomes related to benefits (overall [OS] and disease free/event free survival [EFS/DFS]) and harms (non-relapse mortality [NRM] and graft failure [GF]), independently by two authors. Our search strategy identified 1001 references but only 30 studies (n= 1995 patients) were included in this systematic review/meta-analysis. We also performed a sub analysis on clinical outcomes for studies that included only pediatric patients (defined as <18 years) and those in patients ≥18 years of age.
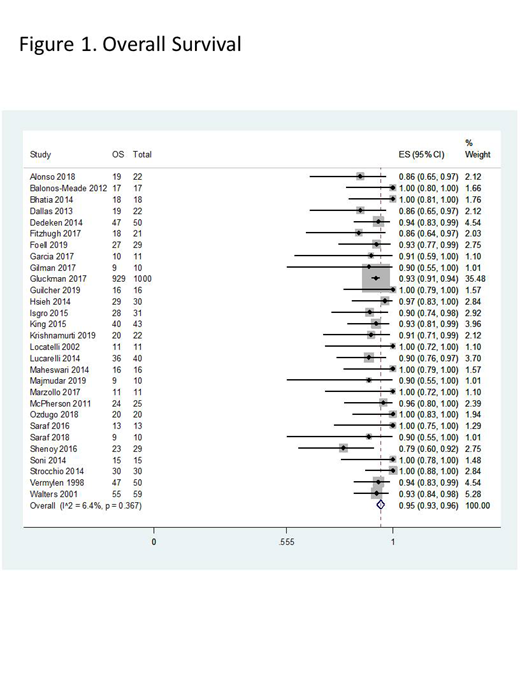
Results: Median age for patients enrolled in all the studies was at 10 years. Recurrent veno-occlusive crises represented the most common indication for allo-HCT followed by acute chest syndrome and stroke; nevertheless, most patients had more than one indication. Matched related donors (MRD) were the most common donor source (93%). Bone marrow was the most common source of hematopoietic stem cells (77%). Majority of patients underwent conditioning with myeloablative regimens (77%). Pooled OS rates (n=29 studies, 1681 patients) after allogeneic HCT was 95% (95%CI=93-96%) with low heterogeneity (I2=6.4%) among included studies (Figure 1). Pooled EFS/DFS rates (n=29 studies, 1894 patients) post-allografting was 90% (95%CI=87-93%) with moderate heterogeneity (I2=54%). Pooled NRM rates from 30 studies (1995 patients) was 4% (95%CI=2-6%) with low heterogeneity (I2=29.4%). Pooled GF rates from 28 studies (1851 patients) was 4% (95%CI=2-6%) with moderate heterogeneity (I2=55%). A subset analysis specifically for pediatric patients (n= 11 studies, 1009 patients, median age at 9.7 years) showed a pooled OS rate of 96% (95%CI=94-97%) with low heterogeneity (I2=0%); and for adult patients (n=3 studies, 51 patients, median age at 33.4 years) the pooled OS was 94% (95%CI=80-100%) with moderate heterogeneity (I2=52%). Pooled EFS/DFS for pediatric patients (n= 11 studies, 1009 patients) was at 89 %( 95%CI=84-93%) with moderate heterogeneity (I2=55.1%); and for adult patients (n=2 studies, 30 patients) was at 95% (95%CI=83-100%) with high heterogeneity (I2=96.5%). Pooled NRM from 10 studies with pediatric patients (281 patients) was at 6 % (95%CI=3-10%) with low heterogeneity (I2=0%); and from 3 studies with adult patients (51 patients) was at 1% (95%CI=0-7%) with low heterogeneity (I2=15.1%). Pooled GF from 10 studies with pediatric patients (281 patients) was at 3 % (95%CI=1-7%) with moderate heterogeneity (I2=40%); and from 2 studies with adult patients (30 patients) was at 5% (95%CI=0-17%) with high heterogeneity (I2=95.4%).
Conclusions:
The results of our systematic review/meta-analysis show excellent OS, EFS/DFS in children and adults undergoing allo-HCT with pooled OS rates exceeding 90%. The main limitation to offering an allo-HCT in SCD remains the availability of a suitable donor as 85% of patients meeting criteria do not have a MRD. We anticipate that with emergence of haploidentical transplantation the number of allo-HCT will increase in the future. GF remains a significant concern in this population and future studies should focus on novel immune suppression strategies to help reduce GF.
Kharfan-Dabaja:Pharmacyclics: Consultancy; Daiichi Sankyo: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal