Background: Improvement in cancer treatment has led to an increase in prevalence of hematological malignancies with a rise in healthcare utilization secondary to this. We aim to identify predictive factors for transfer to another non-acute facility (including nursing home, subacute rehab and other institutional care) at the time of discharge.
Methods: This is a retrospective cohort analysis of NIS database from 2014. Inclusion criteria was any admission of adults (≥18 years) with hematological malignancy (identified by ICD-9-CM diagnosis codes). We identified subgroups of hematological malignancies as follows: multiple myeloma, Hodgkin's lymphoma, non-Hodgkin's lymphoma, acute myeloid and lymphoid leukemia, chronic myeloid and lymphoid leukemias. Patients transferred in from a different acute care hospital or another type of health facility were excluded. Aggressive inpatient care was defined by use of mechanical ventilation, vasopressors, hemodialysis (end stage renal disease excluded) or cardiopulmonary resuscitation. Primary outcome was transfer upon discharge to a different facility excluding acute care hospital (transfer out). Factors associated with this outcome were analyzed using multivariate logistic regression analysis. Statistical analysis was done using STATA.
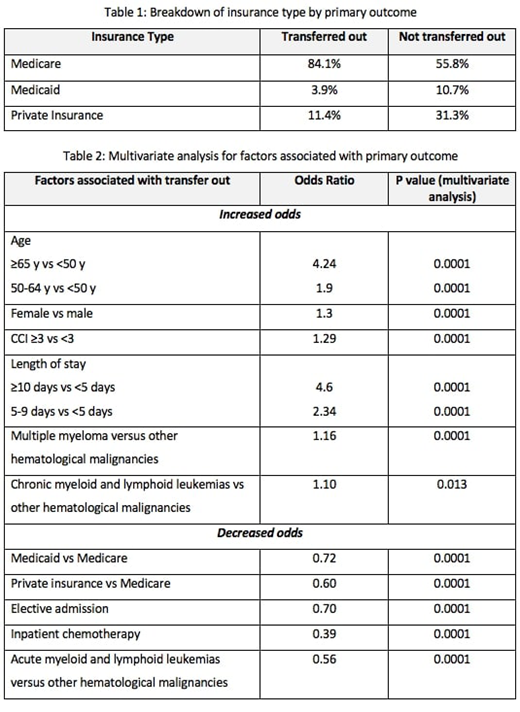
Results: There were 505,230 admissions of patients with hematological malignancy in the year 2014. Of the entire study population, 15.5% (n= 78,390) were transferred out at discharge and the most common primary diagnosis at admission for them was unspecified septicemia. Among those who were transferred out, mean age was 75.4 years (compared to 63.3 years for those not transferred out), mean length of stay was 9.7 days (compared to 6.7 days for those not transferred out) and 75.1% had Charlson Comorbidity Index (CCI) ≥3 (compared to 55.9% for those not transferred out). Also, among those who were transferred out, admission was elective in only 12.6% (compared to 24.9% for those not transferred out), aggressive inpatient care was utilized in 7.8% (compared to 2.1% for those not transferred out) and inpatient chemotherapy was given in 7.2% admissions (compared to 23.3% for those not transferred out). Breakdown of type of insurance for the two cohorts is shown in table 1. Result of multivariate logistic regression analysis for factors associated with primary outcome (transfer out) are summarized in table 2. We adjusted for the factors listed in the table and others such race, mean income quartile of patient's zip-code, hospital factors (urban or rural location, teaching status, geographical region and bed-size) and day of admission (weekend or weekday).
Conclusion: Among admissions of patients with hematological malignancies, older age, female gender, presence of co-morbidities, longer length of stay, diagnosis of myeloma and chronic leukemias were associated with higher odds of transfer to a different non-acute facility at discharge. Whereas, elective admission, insurance type other than medicare, diagnosis of acute leukemias and those receiving inpatient chemotherapy had lower odds of being transferred to a different non-acute facility at discharge. A future area of exploration is development of a scoring system using the most clinically relevant and strongly associated factors to predict risk of transfer to a different non-acute facility at discharge. This will allow early decision making and mobilization of resources by healthcare systems for these patients with complex healthcare needs.
Kuriakose:Alexion: Consultancy, Honoraria, Speakers Bureau; Bayer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal