Introduction: As the complexity of the LYM treatment landscape increases, patients (pts) have become more involved in understanding treatment options, joining advocacy organizations, and seeking information through a multitude of venues. This has increased the pts voice in the treatment decision-making (DM) process while considering several factors (i.e. route of administration, side effects, cost, access to care, quality of life, etc). There is robust evidence that establishes the importance of a collaborative relationship between pts and clinicians when making treatment related decisions. The growing evidence also suggests there is an increased need for pt oriented-research, including communication between the scientific community and cancer pts. However, despite the established need for shared DM, there are discrepancies between the extent that pts prefer to be involved vs their actual involvement. Previous studies have suggested that elderly pts and pts with lower education status prefer a passive DM role. Our objective was to facilitate a detailed survey identifying clinical characteristics and demographics that influence the preferred and actual role that LYM pts have in shared treatment DM.
Methods: This study was reviewed and approved by the Rutgers IRB. A 30 question survey was developed and sent to the LYM Research Foundation (LRF) distribution list of pts and caregivers. This voluntary and anonymous survey was available through the online survey platform Qualtrics®, a Rutgers University approved survey platform, and was sent to 132,827 unique email addresses. Data collection and analysis was performed solely through the Qualtrics online platform with no additional pt identifiers or information collected. Statistical analyses were performed using non-parametric two-sided Mann Whitney U test and Fisher exact testing.
Results: Of the 132,827 unique email addresses that received the survey, an estimated 12,316 recipients opened the email with a total of 1045 participants completing the survey. Among the 1045 participants, 878 were LYM pts or survivors. Of the 878 pts, 58% were current and the remaining were survivors. Among known diagnoses, the most common subtypes were follicular LYM (30%), CLL/SLL (25%), mantle cell LYM (20%), Waldenstroms macroglobulinemia (10%), & diffuse large B cell LYM (8%). At the time of diagnosis, the majority of pts (73.7%) were 60 years or older. There were slightly more female (55%) than male pts. Disease status for pts: 22% had not yet received therapy, 38% reported 1 line of therapy, and 40% 2 or more. Additionally, 49% reported receiving chemotherapy, 55% receiving immunotherapy.
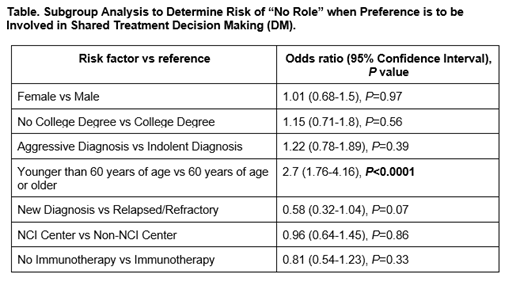
Considering the 878 LYM pts who were included in this analysis, 460 (52%) responded to their preferred role in treatment DM. Furthermore, 448/460 (97%) pts responded that they preferred to have an active role in the treatment DM paradigm. However, 147/448 (33%) responded they did not have a role in the DM process. We analyzed several pt demographic and disease variables for the impact on decision making (Table).There was no significant difference in the probability of pts with no role in DM for most subgroups. There was a trend for LYM pts with relapsed/refractory disease in having less of a role in DM for therapy compared with newly diagnosed pts, while there was no apparent differences based on whether immunotherapy was part of therapy or not. However, there was a prominent difference in the probability of pts when stratified by age with 27% of pts ages ≥60 years vs 50% of LYM pts ages <60 years stating that they did not have a role in DM for their treatment (Table).
Conclusions: This analysis informs the perspective of LYM pts and survivors regarding their roles in treatment DM. While nearly all responding pts reported they preferred to have an active role in the treatment DM process, 1/3 of those pts stated that they did not have a role. This preference transcended most pt demographics and disease characteristics. However, there was a prominent age-based discrepancy with younger LYM pts reporting no role in treatment decisions compared with older pts. Based off of previous evidence that suggests older pts prefer a more passive role, this data suggests pts perception of their actual role in shared treatment DM can be influenced by their reported preference. Continued analyses and studies are warranted to understand the ongoing gaps and to improve the overall DM process for pts and providers.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal