Purpose
Eculizumab is reported to be highly effective in managing patients with paroxysmal nocturnal hemoglobinuria (PNH). However, eculizumab therapy is associated with high cost and thus is inaccessible to all patients with PNH. Additionally, there are some restrictions in the coverage of PNH therapy from the health insurance, which varies depending on each country. In South Korea, majority of the cost involved in eculizumab therapy is supported by the National Health Insurance Service (NHIS) with very limited indication. The patients with PNH must satisfy all of the following criteria to be eligible for financial support from NIHS: (1) PNH granulocyte count ≥ 10%; (2) lactate dehydrogenase ≥ 1.5 times the upper limit of normal; (3) at least 4 units of red blood cells must have be transfused in the past 12 months (transfusion-dependent anemia (TDA)); and (4) exhibit at least more than one of the PNH-related complications (except TDA), which include thrombosis, renal insufficiency, pulmonary insufficiency, or recurrent smooth muscle spasm. These criteria are the narrowest indication for eculizumab therapy compared with those used by other countries. Hence, we performed a nation-wide study including all the patients with PNH in South Korea using the NHIS database to investigate the real-world efficacy of eculizumab.
Methods
The National Health Insurance Database of the NHIS in South Korea was used to collect the data of patients diagnosed with PNH between January 1, 2002 and December 31, 2016. Propensity score (PS) method was used to evaluate the real-world effects of eculizumab on patient survival. For PS method, the patients with PNH were divided into the following two groups: (1) patients treated with eculizumab; and (2) patients not treated with eculizumab. Additionally, the patients used for the analysis were limited to those who are surviving from the time of introduction of eculizumab in South Korea (October 1, 2012). In total, 11 variables were selected for PS matching according to the indications for using eculizumab in South Korea: age, sex, TDA, venous thrombosis, arterial thrombosis, AA, MDS, acute renal failure (ARF), chronic renal failure (CRF), prescription of opioid analgesic drug (≥ 2 times), and pulmonary hypertension. The patients diagnosed with acute leukemia were excluded. The time point of the matching was designated as the date on which the eculizumab was first administered. All survival or complication analyses were performed using the Cox proportional hazard regression model. The duration of PNH was used as the explanatory variable to estimate the proper treatment effect.
Results
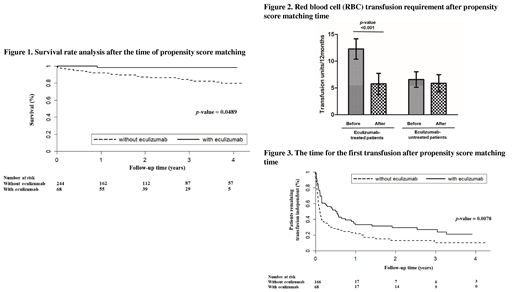
Eculizumab-treated patients exhibited significantly higher survival rate than the eculizumab-untreated patients (4-year survival after propensity score matching, 98.31% vs. 79.67%, p = 0.0489). The mean RBC transfusion units per 12 months after eculizumab therapy was significantly lower than that before eculizumab therapy (5.75 units vs. 12.28 units, p < 0.0001). The median time for the first transfusion in the eculizumab-treated group was significantly longer than that in the eculizumab-untreated group (p = 0.0078). The 4-year transfusion-independence rate for the eculizumab-treated group was significantly higher than that for the eculizumab-untreated group (20.81%; 95% CI, 10.71-33.20%, vs. 10.24%; 95% CI, 4.17-19.50%). There was no significant difference in the incidence of new documented complications related to PNH between the two groups. These complications include venous thrombosis (p = 0.886), arterial thrombosis (p = 0.112), acute renal failure (p = 0.745), chronic renal failure (p = 0.827), use of opioid analgesics (p = 0.142), and pulmonary hypertension (p = 0.396).
Conclusions
Eculizumab therapy for high-risk PNH patients may effectively improve the survival rate and reduce the transfusion requirement. Paradoxically, the eculizumab-treated patients with severe PNH exhibit higher survival rate than the eculizumab-untreated patients with less severe PNH.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal