Introduction: Heparin induced thrombocytopenia (HIT) occurs in up to 5% of adults exposed to heparin due to formation of heparin-dependent antibodies to the heparin/platelet factor 4 (PF4) complex. Patients develop thrombocytopenia and are at risk for severe thrombotic complications. Mortality rates can be as high as 20%, but are often much lower with prompt recognition, cessation of heparin, and treatment with alternative anticoagulants. However, these alternative medications are often both labor-intensive drips and expensive, highlighting the need for quick decision making in such challenging cases. The classic workup of HIT involves assessing clinical suspicion (often using the "4T score" on a scale of 0-8), followed by lab testing for detection of the heparin-dependent antibody and then a functional assay to confirm pathogenicity of the antibody. Our institution uses an in-house rapid Particle ImmunoFiltration Assay (PIFA), which is a same-day test and reported as "positive" or "negative." Other testing available includes send-out tests for Enzyme-Linked Immunoassay (ELISA) to IgG, A, and M of the PF4 antibody as well as the C-14 Serotonin Release Assay (SRA) functional assay. The goal of this retrospective review is to analyze the utility of an algorithmic approach to laboratory testing in aiding the rapidity of diagnosis of HIT without missing possible critical cases.
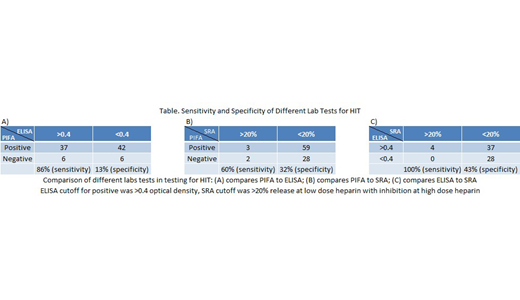
Methods: This was a single institutional study at a large urban academic medical center. We reviewed inpatient charts from 2015-2018 of patients who had any lab testing for HIT. As per institutional guidelines, first-line testing is recommended by using the in-house same-day testing PIFA. If positive, a sample is automatically reflexed and sent-out for PF4 ELISA testing and SRA. Furthermore, clinicians are able to directly order ELISA and SRA testing at their medical discretion. Our analysis looked at those patients with at least two different "HIT-related" laboratory tests to best analyze the concordance and discordance rates of the above testing to assess for sensitivity, specificity, and overall accuracy of using a stepwise testing approach. We used a cutoff value of >0.4 optical density (OD) for ELISA testing, and >20% release at low-dose heparin concentration for SRA testing.
Results: There were 118 patients who had at least two different HIT-related laboratory tests sent. 91 patients had both PIFA and ELISA testing, with 37/79 (47%) positive concordance rate and 6/12 (50%) negative concordance rate, for a sensitivity of 86% and specificity of 13%. 3 patients with positive PIFA also had positive SRA, and there were 2 patients with negative PIFA with positive SRA testing (see attached Table). When comparing ELISA testing to SRA, 4/41 (10%) had concordant positive testing, while no patient with a negative ELISA test had a positive SRA (28 concordant negative cases). Overall, of 94 SRA tests run, 5 were positive, of which 2/5 had negative PIFA and 0/4 had negative ELISA testing.
Conclusions: While PIFA testing had a high sensitivity compared to ELISA, the overall accuracy compared to ELISA was low, while ELISA testing was 100% sensitive in this analysis. Furthermore, there was still a risk of missing cases of HIT using PIFA testing alone. In both cases of positive SRA with a negative PIFA, patients had a high 4T score of >6, consistent with a high clinical suspicion for HIT. We conclude that PIFA testing is not equivalent to ELISA testing, and that use of a laboratory "algorithm only" approach would be inappropriate in the diagnosis of HIT. Our results highlight the importance of using both clinical scoring systems and appropriate lab testing together in the workup and diagnosis of HIT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal