Introduction: Obesity is associated with endothelial dysfunction, hemostatic and fibrinolytic disturbances. The relationship between obesity and elevated Von Willebrand Factor (VWF) is complex and not fully elucidated. There is a significant knowledge gap regarding the impact of BMI on VWF levels. Given the proinflammatory effect associated with abdominal obesity, we hypothesized that there would be an increased prevalence of obesity among individuals with Low VWF (LVWF) compared to Type 1 Von Willebrand Disease (T1VWD) in the ATHN (American Thrombosis and Hemostasis Network) dataset.
Methods: A retrospective review of de-identified patients included in the ATHN dataset as of March 2018 was performed. The dataset was queried for all patients with a diagnosis of "T1VWD," who were over 18 years of age when labs were drawn and when BMI was recorded, who had VWF Ristocetin cofactor (RCO) levels <50 IU/dL and who had BMI entered within 24 months of the date of lab entry. Subjects were categorized with VWF RCO ≤30% as T1VWD and 30-50% as LVWF. We used the NIH definitions for BMI (BMI<18.5, underweight; 18.5-24.9, normal; 25-29.9, overweight; 30-39.9, obese; BMI >40, extremely obese).
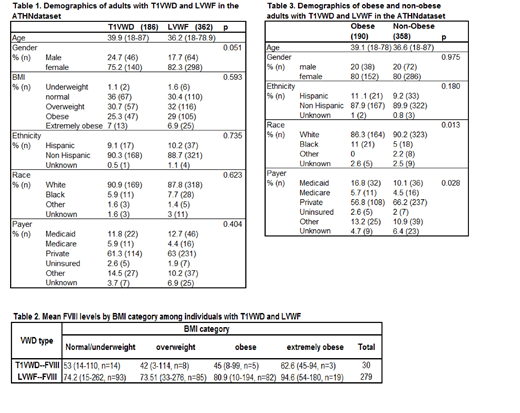
Results: Of the 6939 patients with T1VWD in the ATHN dataset, 4754 patients had VWF RCO <50%, 1019 were above the age of 18, resulting in 548 evaluable subjects with BMI and laboratory metrics. There were 186 patients in the T1VWD cohort, and 362 patients in the LVWF cohort, with a Female:Male ratio >3:1 (Table 1). BMI was treated as a continuous measurement and on bivariate analysis there was not a statistically significant difference (p=0.593), with mean BMI 28.2 (17.2-52) in T1VWD and 28.6 (15.3-55.4) in LVWF. Prevalence of obesity (BMI ≥30) was not significantly different between cohorts (T1VWF 32% vs. LVWF 36%, p=0.345, Table 1). The prevalence of obesity by age (18-39, 40-59, >60 years) was similar among both cohorts with the exception of a larger proportion of obese individuals over the age of 60 in the LVWF cohort (63% vs 25%). Mean FVIII level for LVWF cohort was significantly higher compared to that for T1VWD cohort (80% vs. 53%; p<0.001). In addition, extremely obese patients had an elevated mean FVIII level compared to overweight patients (81% vs. 60%; p=0.041, Table 2).
Among individuals with BMI≥30, there were increased rates for Black race (p=0.013), and Medicaid and Medicare rates (p=0.028) when compared to non-obese individuals (Table 3). While rates of obesity are known to vary regionally, no conclusions could be drawn as there was disproportionate geographic clustering in states with well-established hemophilia treatment centers.
Conclusions: Our analysis identified that 34.8% of adults categorized as VWD in the ATHN data set are obese, with similar prevalence among T1VWD and LVWF. This finding, coupled with associated race, ethnic and socioeconomic risk factors can help prioritize prevention and weight management as a critical component of the comprehensive care model. Increasing degree of obesity may be associated with elevated FVIII, and should be studied prospectively in larger cohorts and the potential impact on cardiovascular risk. Limitations of this analysis include incomplete laboratory data, lack of longitudinal laboratory data, unknown potential confounders including pregnancy or medication effect, and non-uniform geographic distribution of patients. Further research is needed to evaluate the impact of obesity on bleeding phenotype, bleeding related complications, and management practices, as well as the effects of weight change on VWF and FVIII levels.
Schaefer:Siemens: Research Funding; Stago: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal