BACKGROUND: Cerebral sinovenous thrombosis (CSVT) is a rare but serious disease process among all patients, with a slightly higher prevalence in pediatric patients. Despite its low frequency, CSVT represents the second most common type of venous thromboembolism (VTE) in children, next to deep vein thrombosis (DVT) of the limbs. Current literature lacks robust evidence on risk factors for CSVT, especially in the pediatric population. We sought to determine risk factors of CSVT in pediatric patients, via a single-institutional case-control study.
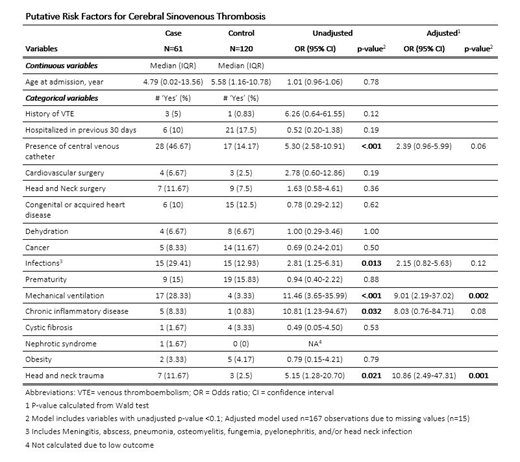
METHODS: A case-control study was conducted at Johns Hopkins All Children's Hospital from patients admitted between March 31st 2006 and April 1st 2018. Cases were identified based on ICD-9 and ICD-10 codes and confirmed via electronic medical record (EMR) review and neuroradiologist confirmation of radiologic testing. Two controls were then randomly selected for each CSVT case, matched by month and year of admission. Clinical and demographic parameters were collected via abstraction from the EMR, including: age at admission, prior history of VTE, previous hospitalization within 30 days, head/neck surgery, other major surgery, congenital or acquired heart disease, dehydration, cancer, serious infection (included meningitis, sepsis, pneumonia, osteomyelitis, fungemia, pyelonephritis, head/neck infection, abscess involving anatomic sites other than skin or head/neck), prematurity, mechanical ventilation, chronic inflammatory disease, cystic fibrosis, nephrotic syndrome, obesity, and head/neck trauma. Associations between CSVT and putative risk factors were evaluated via logistic regression, using odds ratios (ORs) and 95% confidence intervals (95%CIs). Those risk factors with P-values <0.1 in univariate logistic regression were included in adjusted (multivariate) logistic regression modeling; results of the latter employed a threshold of P<0.05 for statistical significance.
RESULTS: A total of 60 CSVT cases and 120 controls were identified. Median (and interquartile range in) age was 4.79 years (0.02-13.56 years) for cases and 5.58 years (1.16-10.78 years) for controls. Factors putatively associated with CSVT in unadjusted analyses were: presence of central venous catheter; serious infection; mechanical ventilation; chronic inflammatory disease; and head/neck trauma. In the multivariate model, mechanical ventilation (OR=9.01, 95%CI=2.19-37.02) and head/neck trauma (OR=11.52, 95% CI=2.63-50.41) remained independent, statistically-significant risk factors for CSVT.
CONCLUSIONS: This single-institutional case-control study reveals that mechanical ventilation and head/neck trauma are independent risk factors for pediatric CSVT. These findings will be further investigated via the multicenter Children's Hospital-Acquired Thrombosis (CHAT) registry dataset, by which a risk model for CSVT in children will be further developed and validated, in order to inform future preventive strategies in pediatric patients at heightened risk of CSVT.
Goldenberg:NIH: Other: research support and salary support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal