Background: A recognized complication of exposure to heparin is the development of heparin-induced thrombocytopenia (HIT) and heparin-induced thrombocytopenia with thrombosis (HITT). The frequency of HIT in patients exposed to unfractionated heparin (UFH) is higher than those exposed to low-molecular-weight heparin (LMWH). Where the use of unfractionated heparin is not necessary, HIT may be largely preventable by using LMWH rather than UFH on an institution-wide scale. At our institution, UFH was largely substituted by the LMWH for thromboprophylaxis gradually throughout 2014 with the implementation of the venous thromboembolism (VTE) thromboprophylaxis protocols. The VTE thromboprophylaxis protocols had their final implementation at the beginning of 2015.
Objectives:
- To determine the incidence of HIT and HITT before and after the implementation of the VTE thromboprophylaxis protocols within Eastern Health.
- ACP Learning Objective: Educate learners about the risk of using UFH as well as alternative treatment for DVT prophylaxis (LMWH).
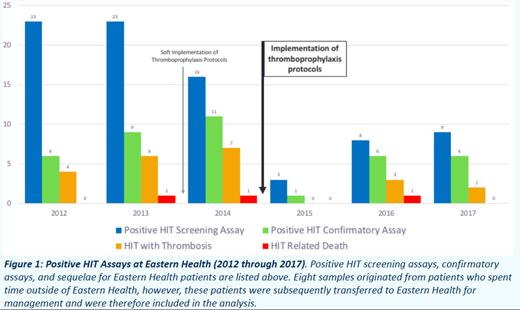
Methods: Charts of all patients who had HIT screening assays requested between January 1, 2012 and December 31, 2017 were examined to determine which patients went on to have positive screening assays as well as positive confirmatory testing. The type of heparin which the patient was exposed was recorded, the sequelae of HITT within 30 days of medication exposure, as well as the correlation of these findings with the implementation of the VTE thromboprophylaxis protocols.
Preliminary Results: In surgical patients the average number of confirmed cases of HIT per year decreased by 51%, and the average number of confirmed cases of HITT per year decreased by 83% after implementation of thromboprophylaxis protocols. In medical patients the average number of confirmed cases of HIT per year decreased by 15%, and the average number of confirmed cases of HITT per year decreased by 47% after implementation of thromboprophylaxis protocols. Between 2012 and 2017 a total of 24 patients experienced HITT, resulting in 33 poor outcomes, including: pulmonary embolism, cerebrovascular accident, DVT, ischemic bowel, arterial thrombosis, venous thrombosis, cardiac thrombus, splenic infarct, and death. The majority of patients experiencing HITT had a history of UFH usage, be it alone or in combination with LMWH, equaling 19 out of 24 patients.
Preliminary Conclusion: The incidence of HIT and HITT was reduced after the implementation of the VTE prophylaxis protocols.
Further Direction: The next step in the project involves assessing the statistical significance of the above results and assessing the data from 2018 in the same manner as above.
Young:Sanofi-Aventis: Honoraria, Research Funding. Chitsike:Sanofi-Aventis: Honoraria, Research Funding; Bayer: Research Funding; Bristol Myers Squib: Honoraria; Pfizer: Honoraria; Servier: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal