Introduction:
The Philadelphia chromosome is associated with a poor prognosis in patients with acute lymphoblastic leukemia (ALL). Prior to the use of hematopoietic stem cell transplantation (HSCT) and tyrosine kinase inhibitors (TKIs), Philadelphia-positive (Ph+) ALL patients were found to have an overall survival (OS) rate of less than 20% over the course of 3 years (Thomas et al., Blood 2004). While modern day therapies including allogeneic HSCT and newer-generation TKIs such as dasatinib have led to significant improvements in OS for this population, these treatments have variable accessibility due to costs for patients with limited to no health insurance.
Methods:
We performed a retrospective study at the Norris Comprehensive Cancer Center and Los Angeles County Hospital, both associated with the University of Southern California, to investigate outcomes in Ph+ ALL adults with different types of health insurance. Individuals included in the study were diagnosed with Ph+ ALL between 2004-2019. Health insurance options included private insurance, Medicare, Medicaid, or no insurance. Treatment modalities included allogeneic HSCT followed by maintenance TKI therapy or combination chemotherapy plus a TKI. The former was preferred if patients met the key transplant eligibility criteria of insurance coverage and caregiver availability at home. Patient OS was defined as the time from diagnosis of Ph+ ALL until patient death. Statistical analysis was performed using the Fisher's exact probability test with two-tailed p-values <0.05 deemed significant.
Results:
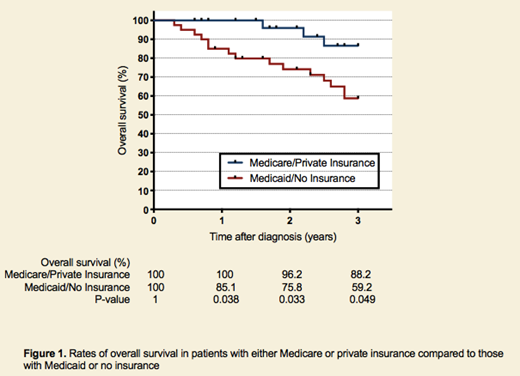
A total of 81 patients with Ph+ ALL were included in this study. Forty-seven patients (58%) were male and the median age at the time of diagnosis was 45 years (range 20-70). Two groups of patients were compared: those with either Medicare or private insurance (M/P) versus those with Medicaid or no insurance (M/N). Thirty-three patients (40.7%) were included in the M/P group and 48 patients (59.2%) in the M/N group. In comparing rates of OS, the 1-year OS was 100% vs. 85.1% (p = 0.038), 2-year OS was 96.2% vs. 75.8% (p = 0.033), and 3-year OS was 88.2% vs. 59.2% (p = 0.049) for M/P patients compared to M/N patients, respectively (Figure 1). In terms of treatment, there was a significant difference in the number of patients eligible to undergo allogeneic HSCT as 20 patients (60.6%) in the M/P group were able to be transplanted in contrast to 15 patients (31.3%) in the M/N group (p = 0.012). There were similar rates of caregiver availability to support HSCT between both groups; 24 M/P patients (72.7%) lived with a caregiver versus 33 M/N patients (68.8%) in comparison (p = 0.806). Furthermore, there were significantly more patients in the M/P group who were able to be treated with the newer-generation TKI dasatinib instead of the older agent imatinib compared to M/N patients (100% vs. 85.4%, p = 0.038).
Conclusion:
With the emergence of allogeneic HSCT and newer-generation TKIs, the rates of OS in the Ph+ ALL population improved dramatically from the prior era (Fielding et al., Blood 2009). However, barriers still exist to receiving these modern therapies, one of the most formidable being sufficient insurance coverage of costs. This study demonstrated that the Ph+ ALL population in the M/P group had significantly higher rates of OS at the 1-year, 2-year, and 3-year marks compared to those in the M/N group. Furthermore, there were also a greater percentage of patients in the former group who were able to undergo allogeneic HSCT during the study period. While eligibility for allogeneic HSCT depended on caregiver availability in addition to insurance status, there were similar rates of caregivers between the two groups, thus implying that this factor had no major impact on the differing rates of HSCT. Dasatinib was previously shown to have increased potency in inhibiting the in vitro growth of cells with wild-type BCR-ABL compared to imatinib, making it a preferred choice for TKI therapy (Li, Leukemia & Lymphoma 2008). There were again significantly more M/P patients than M/N patients who were able to be treated with dasatinib rather than imatinib. Given that health insurance status was found to be correlated with rates of OS, allogeneic HSCT, and the availability of newer-generation TKIs, it remains a critical point of discussion in the treatment of Ph+ ALL patients from all socioeconomic backgrounds.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal