Background About one-half of persons with acute myeloid leukemia have normal cytogenetics but have diverse outcomes which might be explained, at least in part, by specific mutations. We focused on DDX11, the budding yeast ortholog of ChlR1, which encodes an ATP-dependent RNA- and DNA-helicase involved in diverse cell processes such as sister chromatid exchange cohesions and implicated in other cancers and which is associated with telomere shortening.
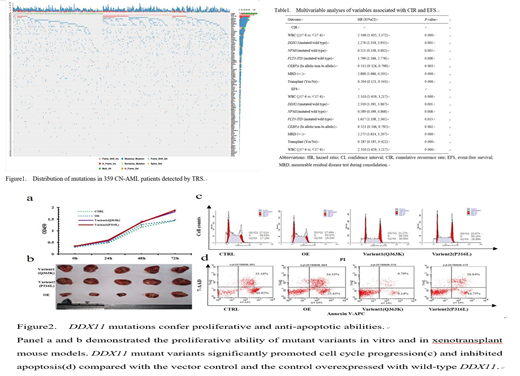
Methods DNA from 359 consecutive, newly-diagnosed adults with AML and normal cytogenetics were interrogated by deep target regional sequencing (TRS). Average effective sequencing depth was 1678.5X (1000.0-1800.0X) and median coverage, 99.9% (98.0, 100.0%). Outcomes studied included cumulative incidence of relapse (CIR) and event-free survival (EFS). DDX11 mutants were transfected into a human AML cell line which was studied in vitro and in immune deficient mice.
Results We identified 2909 non-synonymous somatic variants. 284 subjects (79%; 95% confidence interval [CI], 75, 83%) had ≥5 mutations with a median of 8 mutations per subject (range, 1-20). We identified mutations at 4 new loci including DDX11 in 29 subjects (8%), NPIPA5 in 15 (4%), CYP2F1 in 13 (4%), and MED12 in 9 (3%). In multi-variable analyses DDX11 mutation was independently associated with CIR (Hazard Ratio [HR]= 2.276 [1.318, 3.931]; P=0.003) and EFS (HR=2.319 [1.391, 3.867], P=0.001). Two missense DDX11-mutant alleles (DDX11P316L/WT or DDX11Q363K/WT) were generated and introduced to the kasumi-1 leukemia cells by lentivirus transfection. Both mutants showed proliferative and anti-apoptotic activities in functional analyses and increased resistance to killing by Cytarabine and Daunorubicin in vitro and in transplanted immune deficient mice.
Conclusions Subjects with AML with normal cytogenetics who have a DDX11 mutation have a higher CIR and worse EFS compared with subjects with wild-type DDX11. Functional studies of a transfected DDX11 human AML cell line provide a functional explanation of our clinical findings.
* Correspondence
Profs. Guo-Rui Ruan and Xiao-Jun Huang
Peking University Peoples Hospital and Institute of Hematology
No.11 Xi-Zhi-Men South Street, Beijing 100044, China
T 86-10-88324672
F 86-10-88324672
E ruanguorui@pkuph.edu.cn OR huangxiaojun@bjmu.edu.cn
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal