Background: Cancer patients are at an increased risk for developing venous thromboembolism (VTE). Recent studies, such as the AVERT trial, have shown that primary prophylaxis (PPX) with direct oral anticoagulants (doacs) in high risk cancer patients (Khorana Risk Score (KRS) ≥2) appeared beneficial in preventing blood clots without marked increase in bleeding events (Carrier, et al 2019). However, widespread adoption of this strategy has not yet occurred, possibly due to concerns that the benefit may not be seen in "real life" patients. This study aims to determine, in a community and rural setting, whether the Khorana score predicts risk of VTE in ambulatory cancer patients who are initiating chemotherapy and to compare the absolute risk of VTE and bleeding with results from the AVERT study.
Methods: We conducted a retrospective analysis of adult patients with hematologic or solid tumor malignancies (excluding multiple myeloma) starting a new course of chemotherapy between January 2016 and December 2018. Patients received their treatment at Gundersen Health System (GHS), an independent academic medical center in western Wisconsin, and data was abstracted from the electronic medical record. Patients on continuous anticoagulation were excluded. KRS was calculated for each patient based on individual values obtained prior to starting treatment. The medical record was reviewed for documentation of VTEs and bleeding events from the time of chemotherapy initiation through 180-days of treatment. Statistical analysis included the use of Chi-Square and Fisher's Exact tests, multivariate logistic regression and Kaplan-Meier analysis.
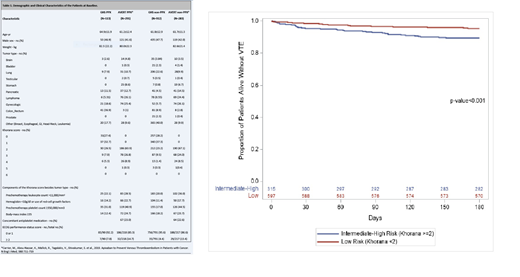
Results: 1,025 patients were identified who fit the inclusion criteria. Demographics are shown in table 1, with comparisons to the AVERT study population. At the time of chemotherapy initiation, 35% (n=360) of our patients had a Khorana score of ≥2 and would have been eligible for PPX based on the AVERT study. 113 total patients received PPX per treating physician recommendation (int/high risk KRS n=45, low risk KRS n=68). Enoxaparin was most commonly used as prophylaxis (88%) while doacs were used in only 12.7%. Of those who did not receive prophylaxis, we found that KRS ≥2 was associated with significantly shorter VTE-free survival (graph 1). Patients in this group had 2.38-fold higher odds of developing a VTE compared to those with a score of 0-1 (p=.0012). In patients who received prophylaxis, the KRS was no longer predictive (p=0.87). In high risk patients without prophylaxis the probability of thrombosis within 180 days was 10%, nearly identical to that seen in the AVERT trial control arm (10.2%). Likewise, the bleeding event rate was similar at 2.4% compared to 1.8%. Of patients who received prophylaxis, the rates of bleeding (2.2 vs. 3.5%) and clotting (6.7 vs 4.2%) were also similar to the PPX arm of the AVERT study.
Conclusions: In a community/rural setting, our population of cancer patients initiating chemotherapy showed a nearly identical risk of both VTE and bleeding as compared to the published clinical trial data. The KRS was able to predict the risk of VTE in our patients and stratify them into a higher risk subset, who may benefit from prophylaxis. In evaluating the patients for whom PPX was prescribed, it does not appear that the KRS was used in the decision-making process, as the majority who received PPX were in the low risk category. Given the published number needed to treat (17) and number needed to harm (100) with apixaban prophylaxis, widespread application of a prophylactic strategy to our patient population may have prevented 21 VTEs and led to 4 additional bleeding events. This risk to benefit ratio appears favorable. While this analysis does not consider important factors like patient preference, provider preference, and cost, it certainly does lessen concerns that our patients are significantly different from those that benefited from prophylaxis in the clinical trial. We plan on using this data to begin a KRS-based risk stratification approach to VTE prophylaxis in our cancer patients starting chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal