Intoduction
Hematological malignancies are often complicated by secondary immunodeficiency (SID), namely hypogammaglobulinemia, the cause of common and opportunistic infections, which represent the major morbidity aitiology for hematological patients (pts)(Friman V, et al. Hematol Oncol 34: 121-132, 2016). Immunoglobulin replacement with intravenous gamma globulin (IVIg) reduces the number of infections, antibiotics' need and hospitalization days (Raanani P, et al. Leuk Lymphoma 50(5): 764-772, 2009). The subcutaneous (sc) route of IgG although equally effective, presents certain constraints (reduced bioavailability, multiple injection sites, and frequent infusions). The facilitated subcutaneous immunoglobulin (fSCIg) method exploits the pharmacologic properties of recombinant human hyaluronidase (rHuPH20) and has been studied in primary immune deficiency (PID) syndromes with similar efficacy to IVIG (Wasserman RL. Immunotherapy 6(5): 553-567, 2014). fSCIg has demonstrated several advantages; self-administration, same bioavailability, long infusion intervals, few adverse drug reactions-ADRs. However, fSCIg has been less extensively studied in SID.
Aim
We present our single-center real-world data from fSCIg administration in hematological pts with SID, focusing on safety and efficacy issues.
Patients and Methods
Since 14-Oct- 2015 fSCIg has been used as the primary immunoglobulin reconstitution treatment (IgRT) in our department for hematological pts fulfilling the ESMO 2015 guidelines (Eichhorst B, et al. Ann Oncol 26(5): v78-v84, 2015): hypogammaglobulinemia with recurrent bacterial infections. No PSAF (proven specific antibody failure) is performed before IgRT initiation. Treatment goal is IgG trough levels around 600 mg/dL. The fSCIg(10% IgG) dosage is 0.4-0.8 g/Kg/month. Treatment modifications are made according to infection occurrence. fSCIg is administered with a variable rate portable pump and a sc 24G needle . First, pts receive rHuPH20 (1-2 ml/min). Ten min after rHuPH20, fSCIg(10%) is infused through the same sc needle, at the same injection site. The rate of the 1st fSCIg infusion is gradually increased from 10ml/h to 300 ml/h. If well tolerated, pts are treated with the final rate of 300 ml/h for subsequent infusions. The first 5 infusions take place at our department and the pts/relatives are instructed how to use the pump. The subsequent infusions take place outside hospital facilities. IgRT is given indefinitely to this pt population.
Results
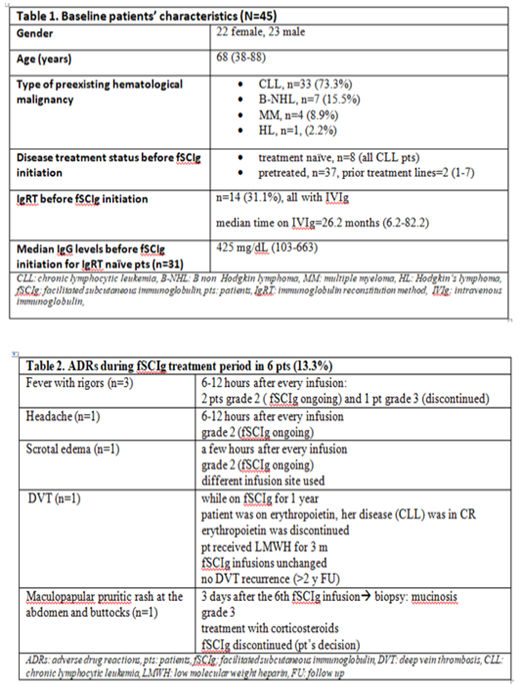
Between mid-October 2015 and mid-July 2019, 45 hematological pts have been treated with fSCIg(10%) at our department according to ESMO 2015 guidelines. Baseline pts' characteristics are shown in table 1. Nine hundred sixty-two (962) infusions were administered, with median number of infusions per pt 19(3-48), median time on treatment 23.5 months(1-44.8) and median follow up 23.9 months (1.4-44.8). Thirty-nine (39) pts (86.7%) were able either to self-administer the formulation or to be treated by the aid of a relative after the 5th training session. More than 700 infusions were performed outside hospital's facilities. Thirty-nine (39) pts (86.7%) had no adverse drug reaction- ADR-, except mild edema at the site of injection for 8-24 hours after the infusion. Six patients (13.3 %) presented at least one type of ADR (table 2). In 11 pts (24.4%) at least 1 infection episode was noticed. All cases were grade 2, except an appendicitis case (grade 3) that it was surgically managed. There were 4 cases of upper respiratory tract infection, 3 cases with lower respiratory tract infections, 2 dermal infections and 1 viral gastroenteritis. fSCIg dose modification was done in 3 pts.
During the follow up period 37 pts (82.2%) are ongoing and 8 pts (17.8%) have discontinued fSCIg: 6 due to death from underlying malignancy and 2 (4.4%) due to ADRs (1 with grade 3 rash and 1 with grade 3 fever and rigor). Surprisingly, there was no death from infectious complication.
Conclusions
Our single-center real-world data from fSCIg administration in hematological patients with hypogammaglobulinemia and recurrent infections shows that this method is very effective in reducing infections, with few ADRs. These findings compare favorably to those observed with IVIg (Raanani P, et al. Leuk Lymphoma 50(5): 764-772, 2009). Finally, fSCIg reduces the nursing staff workload in hematology wards and is preferred by the vast majority of the patients.
Panayiotidis:Bayer: Other: Support of clinical trial.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal