Background: Recurring mutations have been identified in acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) which translate to therapeutic targets. Isocitrate dehydrogenase-1 and -2 (IDH1/2) mutations occur in ~20% of AML, and up to 12% of patients with MDS. Three conserved mutational hotspots in the IDH enzymes alter their function and lead to the production of (R)-2-hydroxyglutarate (2HG), an oncometabolite with numerous downstream effects, including impaired DNA damage repair. Specifically, homologous recombination (HR) is impaired by inhibiting the function of histone demethylases that are critical for HR and recruitment of the HR machinery to sites of DNA damage. In HR deficient tumors poly-ADP ribose polymerase (PARP) enzymes mediate a key salvage pathway. PARP inhibition in HR deficient tumors leads to synthetic lethality via simultaneous inhibition of HR and SSB mediated DNA repair. Our group previously demonstrated synthetic lethality with PARP inhibition in IDH mutant cells lines, and other IDH mutant models including primary patient-derived cell lines and genetically-matched tumor xenografts.
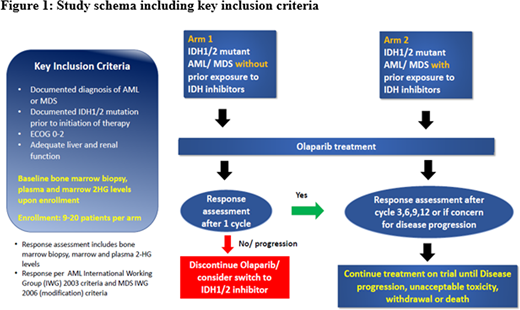
Study Design andMethods: The PRIME trial (NCI10264) is a proof of concept, biomarker-driven, multi-institution, phase II open label clinical trial to assess the overall response of IDH1/2 mutant relapsed/refractory AML and MDS to PARP inhibitor monotherapy with olaparib. The clinical trial is executed by the Experimental Therapeutics Clinical Trials Network of the NCI. The Cancer Therapy Evaluation Program will provide olaparib. Eligibility criteria include documented IDH1 or IDH2 mutation in blood or bone marrow within 30 days of enrollment based on mutational testing by PCR or sequencing in a CLIA certified laboratory and willingness to undergo a bone marrow biopsy. Patients will be treated with olaparib 300 mg q12hrs each day of a 28-day cycle, using a tablet formulation, until disease progression, unacceptable toxicity, withdrawal of consent or death. Blood and bone marrow samples for 2-HG analysis will be collected prior to starting therapy and after 1 cycle (28 days), cycle 2, 3, 6, 9, 12 or when there is concern for disease progression (Figure 1).
A Simon two-stage optimal design will be used to test the null (ORR=10%) versus the alternative hypothesis (ORR=40%) in each arm. In the first stage, 9 patients will be accrued in each arm. If one or fewer responses are observed in these 9 patients, that arm will be stopped early for futility. Otherwise, 11 additional patients will be accrued for a total of 18 in each arm. We reject the null hypothesis if at least 5 responses are observed in these 20 patients. In each arm, we have approximately 90% power to detect a 30% increase in ORR at a one-sided type I error rate of 0.05.
Primary endpoint: Overall response rate (ORR) of 40%, i.e., a 30% ORR improvement (40% vs. historical control ORR = 10%) based on MDS International Working Group 2006 criteria and AML MDS International Working Group 2003 criteria after 6 cycles of treatment. Cumulative ORR will include complete remission, complete remission with incomplete blood count recovery, partial response, and bone marrow complete remission.
Secondary endpoints: Progression-free survival (the interval between the time of initiation of olaparib to the time of documentation of olaparib failure or last follow-up) and overall survival (the interval between the time of initiation of olaparib to the time of death or last follow-up) for the trial.
Exploratory studies: The PRIME trial will also test the utility of 2-HG and DNA damage markers such as γ-H2AX as potential biomarkers of response to olaparib. Using multiple viability assays on leukemia cell lines and bone marrow cultures we will assess synergistic therapeutic combinations to further improve outcomes in this patient population. To confirm efficacy in vivo without undue toxicity, promising combination therapies will be confirmed in cytokine-humanized immunodeficient "MISTRG" mice. We will also examine the impact of PARP inhibitors on the genomic, proteomic, metabolomic and immunologic landscape of IDH 1/2-mutant hematologic malignancies using DNA whole exome sequencing (WES), RNA-Seq, and liquid chromatography-mass spectrometry assessment of oncometabolites.
Bindra:Cybrexa: Consultancy, Equity Ownership. Prebet:pfizer: Honoraria; pfizer: Honoraria; pfizer: Honoraria; Boehringer Ingelheim: Research Funding; pfizer: Honoraria; Tetraphase: Consultancy; novartis: Honoraria; novartis: Honoraria; Genentech: Consultancy; Boehringer Ingelheim: Research Funding; novartis: Honoraria; Boehringer Ingelheim: Research Funding; Agios: Consultancy, Research Funding; Jazz Pharmaceuticals: Consultancy, Honoraria, Research Funding; pfizer: Honoraria; novartis: Honoraria; Bristol-Myers Squibb: Honoraria, Research Funding; novartis: Honoraria.
We will be using PARP inhibitors as a novel therapy for patients with relapsed or refractory AML and high risk MDS based on preclinical data.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal