[Background] Patients treated with immunosuppressive drugs for autoimmune diseases may suffer "other iatrogenic immunodeficiency-associated lymphoproliferative disorders" (OIIA-LPD). Some OIIA-LPDs regress after drug withdrawal but others need cytotoxic chemotherapy. However, the factors associated with a response to drug cessation remain unknown.
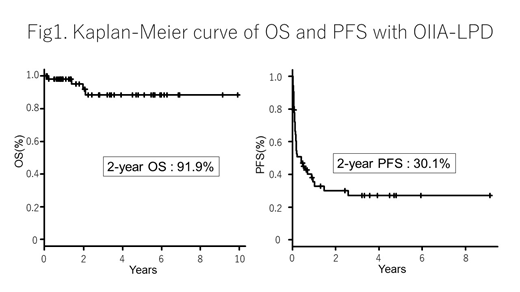
[Methods] We collected clinical data on OIIA-LPD diagnosed between 2009 and 2018 at the University of Tsukuba Hospital and Toranomon Hospital in Japan. Clinicopathological features were retrospectively analyzed. The probability of overall survival (OS) and progression-free survival (PFS) was calculated using the Kaplan-Meier method. OS was defined as the time between the date of diagnosis of OIIA-LPD and the date of death or last follow-up. PFS was defined as the time from the date of diagnosis of OIIA-LPD to the date of commencing chemotherapy or the date of death or last follow up.
[Results] Fifty-four cases of OIIA-LPD were identified, of which 25 were diagnosed at the University of Tsukuba Hospital and 29 at Toranomon Hospital. The male to female ratio was 1:3.5 and the median age at diagnosis was 70 years (range, 35-85). Thirty-four patients (63%) had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Most patients (n=50 [93%]) had rheumatoid arthritis (RA). The remaining 4 patients had systemic lupus erythematosus (SLE), myasthenia gravis (MG), polymyalgia rheumatica (PMR), and polymyositis (PM), respectively. Methotrexate (MTX), tacrolimus, and biological agents were used in 49, 17, and 16 cases, respectively. Histological diagnoses of OIIA-LPD type were diffuse large B-cell lymphoma (DLBCL) (n=24), composite lymphoma of DLBCL and follicular lymphoma (FL) (n=1), Hodgkin lymphoma (HL) (n=18), MALT lymphoma (n=2), peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS) (n=2), angioimmunoblastic T-cell lymphoma (AITL) (n=1), B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and classic HL (n=1), extranodal NK/T-cell lymphoma (ENKTL) (n=1), Burkitt lymphoma (n=1), and not specified (n=3). Epstein-Barr virus (EBV) was detected in 61% of cases tested (31/51) by in situ hybridization for EBER. At diagnosis of OIIA-LPD, 44 cases (81%) were under MTX treatment. MTX was discontinued in all of these, after which spontaneous regression was observed in 27 (61%). There was no clinical response in 5 patients (11%) within 2 months of MTX cessation, and 12 patients (27%) received chemotherapy without confirming whether stopping MTX would have been sufficient intervention. In 27 cases with spontaneous regression after cessation of MTX, 18 achieved complete remission without chemotherapy, but 9 needed chemotherapy due to re-initiation of LPD. Regarding the histological diagnosis, spontaneous regression was observed in OIIA-LPD patients with DLBCL in 12 of 24 cases (50%) and those with HL in 8 of 18 (44%). After achieving spontaneous regression, patients with DLBCL (10/12 cases, 83%) did not require any form of chemotherapy more often than those with HL (4/8 cases, 50%). Neither EBV positivity nor histology were associated with spontaneous regression. With a median follow-up of 26.1 months (range, 1-120.7), 2-year OS and PFS was 91.9% and 30.1%, respectively. The 2-year PFS of DLBCL and HL was 33.1% and 17.5%, respectively (p=0.533). Only four patients died due to the progression of OIIA-LPD.
[Conclusion] Fifty-four cases of OIIA-LPD were retrospectively analyzed. Spontaneous regression after MTX discontinuation was observed in approximately 60% of these patients. No factors associated with response to drug cessation were associated with histological features or EBV positivity, but patients with DLBCL remained in complete remission more frequently than those with HL. Despite the fact that 2-year PFS is low, our retrospective analyses revealed favorable OS of OIIA-LPD because chemotherapy resulted in a good response regardless of whether MTX discontinuation was effective.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal