Introduction: Diffuse large B-cell lymphoma (DLBCL), the most common subtype of non-Hodgkin lymphoma (NHL), is strongly correlated with virus infection and host immunity status. To date, several kinds of virus infection have been involved in the tumorigenesis and progression of NHL, such as Epstein-Barr virus, hepatitis C virus, human immunodeficiency virus and so on. Hepatitis B virus (HBV) infection is a significant public health problem around the world, especially in China. HBV infection has been found to have an epidemiologic association with NHL and HBsAg status has been shown to be associated with the clinical feature and prognosis of DLBCL patients. However, no literature has been reported regarding the effect of HBV antibody in DLBCL. This study was to evaluate the impact of HBV antibody status on clinical outcome and prognosis in DLBCL patients.
Methods: In this retrospective study, we investigated the clinical data of 190 patients with newly diagnosed and untreated DLBCL, who had received histological diagnosis and standard treatment at Shandong Provincial Hospital from May 2013 to May 2018. 127 DLBCL patients were effectively followed up to September 2018. Various statistical analyses were used to determine the significance of HBV antibody status in DLBCL patients.
Results:
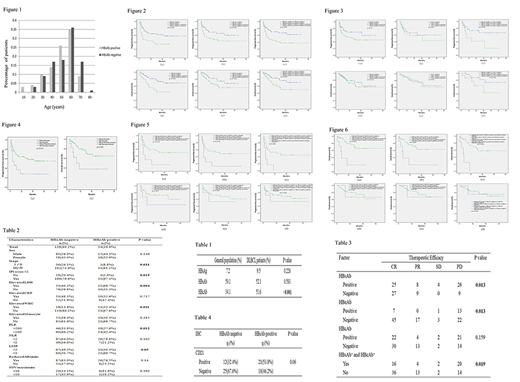
The prevalence of HBsAg, HBsAb and HBcAb were increased in DLBCL patients compared with that in general Chinese population (Table 1).Compared with HBeAb-negative patients, HBeAb-positive patients displayed unique clinical features, such as more advanced disease stage (p=0.031) and higher International Prognostic Index (IPI) score (p=0.015, Table 2). Besides, patients in HBsAb-positive group displayed younger onset age (Figure 1).
Patients in HBV antibody-negative group had better therapeutic efficiency than the positive group (Table 3), including HBsAb (p=0.013), HBeAb (p=0.013), combined HBsAb and HBcAb (p=0.019). The media progression-free survival (PFS) of HBeAb-positive group (p=0.004), HBcAb-positive group (p=0.038), HBsAb-positive and HBcAb-positive group (p=0.008) and the media overall survival (OS) of HBeAb-positive group (p=0.007), HBcAb-positive group (p=0.103), HBsAb-positive and HBcAb-positive group (p=0.035) were shorter than the negative group, respectively (Figure 2). We found the positive association between the expression of CD21 and HBsAb status (p=0.06, Table 4), both of which had no statistical significance in prognostic prediction. However, the media PFS (p=0.035) and OS (p=0.079) of patients with positive HBsAb and positive CD21 expression were worse than the negative group (Figure 3).
Patients in Rituximab-containing group had better therapeutic efficiency (p=0.05), better PFS (p=0.015) and OS (p=0.008) than patients in Rituximab-free group (Figure 4). Interestingly, there were significant differences of Rituximab effect on clinical prognosis depending on the status of HBV antibody (Figure 5 and 6). For example, the positive effect of Rituximab on PFS (p=0.019) and OS (p=0.001) in HBsAb-positive patients was statistically significant while no difference was observed in PFS (p=0.251) and OS (p=0.987) in HBsAb-negative patients. In HBcAb-positive group, patients with Rituximab had better PFS (p=0.019) and OS (p=0.004) than patients without Rituximab. However, for HBcAb-negative patients, the PFS (p=0.596) and OS (p=0.80) were similar in Rituximab-containing group and Rituximab-free group. Similarly, the PFS (p=0.004 vs p=0.479) and OS (p<0.001 vs p=0.936) according to the use of Rituximab displayed significant difference in HBsAb-positive and HBcAb-positive group rather than the negative group.
Conclusions: The prevalence of HBV was increased in DLBCL patients and patients with positive HBV antibody displayed unique clinical features. Our investigations identified for the first time that HBV antibody had a negative effect on clinical outcome and prognosis in DLBCL patients. Interestingly, the effect of Rituximab in prognostic prediction was more significant in HBV antibody-positive group than the negative group. Therefore, our findings lead to a novel understanding of the association between HBV antibody and DLBCL development and provide promising factors for the prognostic prediction in DLBCL patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal