INTRODUCTION. Chromosome banding analysis (CBA) is the gold standard to identify complex karyotypes (CK; ≥3 chromosomal aberrations in the same clone). CK are predictors of poor prognosis and treatment refractoriness in patients with chronic lymphocytic leukemia (CLL). Patients with CK (15% at diagnosis) constitute a heterogeneous subgroup with highly variable clinical course. Recent studies that aim to refine CK definition in CLL suggest that ≥5 is the number of anomalies detected by CBA that better predicts an impaired outcome (Baliakas et al, 2019). Molecular techniques as genomic microarrays also detect genomic complexity (GC). A recent multicentric ERIC study (Leeksma et al, ASH 2017) identified that patients with ≥5 copy number alterations (CNA) detected by microarrays are associated with an adverse outcome. However, risk stratification regarding genomic complexity assessed by CBA and microarrays has not been compared.
OBJECTIVES. 1. To compare genomic complexity in CLL defined by CBA vs microarrays; 2. To compare risk stratification based on genomic complexity measured by both techniques.
METHODS. The study cohort included 293 CLL patients from 16 European institutions (67% males) with available CBA result at diagnosis or prior to first treatment. The cohort was enriched in patients with CK (n=153, 52%). Tumor DNA extracted from peripheral blood (n=254) or bone marrow samples (n=39) obtained at the time of CBA was hybridized to CGH-arrays (n=12) and SNP-arrays (n=281) platforms. Clinically relevant aberrations [11q-, +12, 13q-, 17p-] and CNA ≥5Mb were considered for the anomaly count. Three risk groups were defined using previously suggested cut-off points for CBA and microarrays [non-CK/low-GC: 0-2; low/intermediate-CK/GC: 3-4; high-CK/GC: ≥5 (Baliakas et al, Leeksma et al)]. Groups obtained by both methods were compared and correlated with other clinical and biological data. Time to first treatment (TTT) of patients categorized according to the number of alterations detected by CBA and microarrays was analyzed.
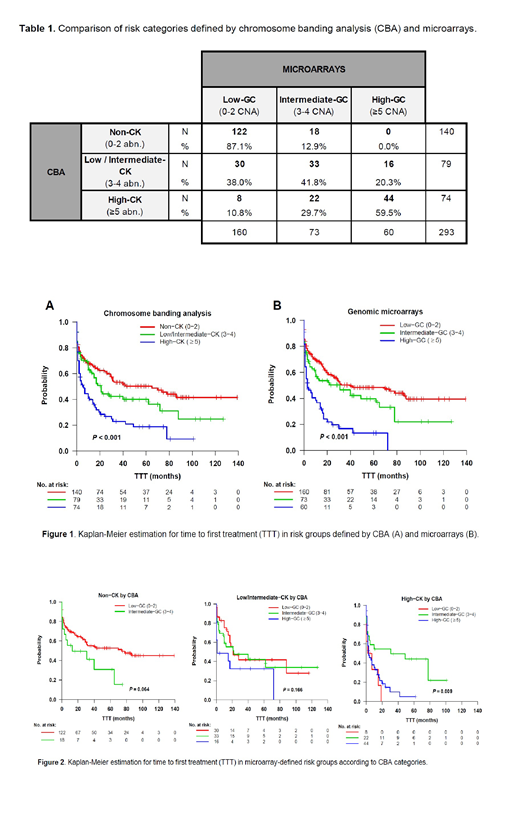
RESULTS. Median number of abnormalities detected was 3 (range: 0-19) by CBA and 2 (range: 0-18) by microarrays. When stratified according to previously defined criteria, a moderate agreement was observed between both techniques (κ=0.483, p<0.001). Remarkably, 8/74 (11%) of patients with high-CK were considered low-GC by microarrays while none of the 140 patients with non-CK was classified as high-GC by microarrays (Table 1). Discordances in those 8 cases underestimated by microarrays were due to the presence of chromosome markers or complex rearrangements in the karyotype which were globally balanced or to subclonal aberrations expanded during CBA culture but represented in a minor proportion of the whole sample.
Regarding the prognostic value of genomic complexity and considering the number of abnormalities detected as a continuous variable, CBA and microarrays showed a similar concordance index (C-index) for TTT (0.615 vs 0.609, respectively). When considering all the abnormalities independently of their size or when lowering the cutoff to 1Mb for those non-CLL abnormalities, similar impact on TTT was observed (C-index=0.593 vs 0.616). The three risk groups defined by each method showed significant differences on TTT (Figure 1, p<0.001). In discordant cases, significant differences on TTT were only observed in cases with high-CK, where low-GC and high-GC showed poor outcome when compared to intermediate-GC group (Figure 2, p=0.009). As genomic complexity category increased in both techniques, a significant increment of del/mutTP53 (CBA: 13% vs 29% vs 62%, p<0.001; microarrays: 16% vs 26% vs 68%, p<0.001) and unmutated IGHV (U-IGHV) (CBA: 49% vs 59% vs 71%, p=0.015; microarrays: 47% vs 68% vs 73%, p=0.001) cases was observed. Of note, among the 8 high risk patients underscored by microarrays, 3 showed del/mutTP53 and 6 showed U-IGHV. Additional techniques, as chromosome painting, are ongoing to confirm microarray results and find an explanation for discordances.
CONCLUSIONS. 1. CBA and microarrays are helpful techniques for assessing genomic complexity in CLL patients; 2. Risk categories established by both methods have a significant impact on TTT although they show a moderate agreement; 3. Discordant cases are being investigated to refine genomic complexity criteria equivalent by both techniques.
ACKNOWLEDGEMENTS. 17SGR437, GLD17/00282, FPU17/00361
Rigolin:AbbVie: Speakers Bureau; Gilead: Speakers Bureau; Gilead: Research Funding. Gimeno:JANSSEN: Consultancy, Speakers Bureau; Abbvie: Speakers Bureau. Bosch:Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; AstraZeneca: Honoraria, Research Funding; Takeda: Honoraria, Research Funding; F. Hoffmann-La Roche Ltd/Genentech, Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Acerta: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Kyte: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Celgene: Honoraria, Research Funding. Cuneo:Amgen: Honoraria; Abbvie: Honoraria, Speakers Bureau; Gilead: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Roche: Honoraria, Speakers Bureau. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal