Introduction:
Sickle cell disease (SCD) is an inherited blood disorder with significant healthcare resource utilization in the United States (US). The clinical management throughout the course of the disease is variable. Children born with SCD in the US receive routine comprehensive care that significantly reduces their morbidity and mortality. Upon transition to adulthood, there are marked increases in disease-related complications and morbidity. The extent to which disease management costs vary by age and overall lifetime cost of treatment are unknown. The aim of this study is to estimate the total direct healthcare cost among patients with SCD in the US across consecutive age ranges.
Methods:
We estimated direct costs of chronic management for SCD through a retrospective database analysis of Optum's de-identified Clinformatics® Data Mart Database (CDM) commercial insurance medical and pharmacy claims from January 1, 2007 to December 31, 2017. CDM provides information on 15 to 18 million annual insured lives and roughly 57 million unique lives over our study period (2007-2017). The population spans 50 states and is similar to the US distribution with respect to sex, age, and geography.
We identified patients using ICD-9-CM (282.4x or 282.6x) and ICD-10-CM (D57.x sans D57.3x) diagnosis codes. Patients were required to have at least one inpatient (IP) claim or three or more outpatient (OP) claims (spaced at least 30 days apart) with a diagnosis of SCD and minimum of one year of continuous enrollment in both medical and prescription drug coverage. Each patient's index date was designated the date of their first SCD-related claim for patients with SCD, or their first date of eligibility for patients without SCD (controls).
We matched patients with SCD to controls using 1:1 propensity score matching without replacement with a greedy nearest neighbor algorithm. Propensity scores were generated using probit regression on covariates gender, state, plan type, year of birth, and index year. Total direct costs of healthcare including IP, OP, professional (PF), ancillary (AN), and pharmacy (RX) services were calculated first year post-index (Y1), second year post-index (Y2), third year post-index (Y3), and overall (annualized) post-index. We calculated annualized costs by aggregating all costs after index and dividing by the remaining number of years the patient was eligible for coverage. Average incremental costs (AIC) are defined as the mean difference in costs between patients with SCD and respective controls. We report AIC by decade of age on the patient's index date, inflated to 2018 US dollars. All analyses were performed in SAS 9.4 (SAS Institute, Raleigh, NC) and Stata 16.0 (StataCorp, College Station, TX). This study was approved by the University of Southern California's University Park Institutional Review Board (UPIRB).
Results:
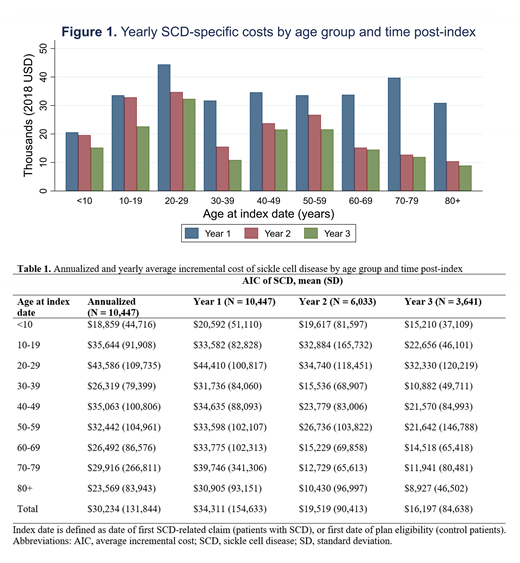
We identified 10,447 patients with SCD along with 10,447 unique matched controls from 2007 to 2017. Average total costs (sum of IP, OP, PF, AN, and RX costs) for patients with SCD were greater at all age categories, relative to controls. Annualized AIC, i.e. costs attributable to management of SCD, ranged from $18,859 (SD = 44,716) for ages 0-9 to $43,586 (SD = 109,735) for ages 20-29 (Table 1). First-year AIC were consistently greater than second and third-year AIC across all age groups (Figure 1). For patients with SCD, AIC were greatest for patients in the 20-29 years band across all specifications. Details on AIC of SCD management across all consecutive age ranges are available in Table 1.
Conclusions:
The cost of disease management for patients with SCD in the US is substantial. We observe a rise in SCD-specific costs from childhood to early adulthood. This may reflect the higher risk of disease-associated complications and mortality seen during this period. Additionally, AIC first year after initial SCD-related claim are consistently higher compared to AIC in years two and three. This finding may be attributable to an increased utilization of healthcare services from previously underinsured patients with SCD. Future work should involve simulating estimated lifetime total direct cost of healthcare attributable to management of SCD for patients in the US.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal