Introduction
Improvements in overall survival (OS) and quality of life (QoL) are clinically relevant outcomes that should guide clinical decision-making. Patients with MPNs can live with their disease for a long period of time, which increases the importance of understanding the impact of treatment in regards to a patients' Health-Related QoL. Therefore, including PROs in clinical trials has become paramount in facilitating informed treatment decisions made by health care providers and patients. Furthermore, the FDA encourages the implementation of patient-centric measures in clinical trials.
Objective
We aimed to evaluate the frequency at which PRO measures are utilized as study endpoints and are made publicly available when trial results are published.
Methods
A review was conducted to characterize studies that have evaluated PRO in patients undergoing treatment for myeloproliferative neoplasms. We searched Citeline® Trialtrove database, a registry of clinical trials, for randomized clinical trials including patients with all myeloproliferative neoplasms, initiated between the years 2006-2016, utilizing at least 1 PRO. We excluded trials that evaluated supportive care and studies with no publications. For included trials, we recorded the following data: indication, treatment and comparator, clinical development phase, endpoints, trial sponsorship, and type of scale or questionnaire used for PRO endpoint. We then identified all available publications associated with the trial, and recorded type of publication (abstract or full text), year, number of randomized patients, and reported outcomes.
Results
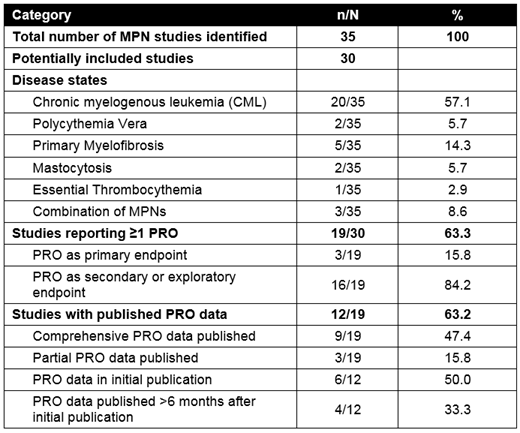
Thirty-five MPN trials were obtained through our search. Trials included patients with chronic myelogenous leukemia (CML), polycythemia vera (PV), essential thrombocythemia (ET), primary myelofibrosis, and mastocytosis. Of these 35 trials, 16 were excluded; two studies were classified as supportive care, three studies did not have a publication or were terminated without results, and 11 studies did not have at least one PRO. 19 trials (19/30; 63%) included at least one PRO assessment as an endpoint and were included in the analysis. Among these 19 trials, the commonly used PRO assessments were EQ-5D, EORTC-QLQ C30, Total Symptom Score (TSS), FACT-Leu, FACT-G, MPN-SAF, and Patient Global Impression of Change (PGIC). Three of the 19 trials (15.8%) utilized at least one PRO as a primary endpoint. Among the 19 trials, thirteen (68.4%) were sponsored by industry, three (15.8%) were sponsored by industry-academic collaborations, and three (15.8%) were sponsored solely by academic institutions. 12 studies (63.2%) reported PRO results within their publications. Six studies (31.6%) reported PRO data within their initial publication. Nine of the19 trials (47.4%) included a comprehensive report of PRO data within their publications, while three (15.8%) only partially reported PRO data. Of the 12 trials with published PRO data, four of 12 (33.3%) reported the PRO more than six months after the initial full publication. Most of the included trials focused on disease control outcome and overall survival benefit was not shown.
Conclusions:
Despite a growing emphasis on QoL and the inclusion of PROs in oncology clinical trials, a significant number of the observed MPN randomized trials did not include a PRO measure. Of those trials that included a PRO measurement, many lacked the comprehensive reporting needed to inform the assessment of clinical benefit and respective decisions. Early and timely reporting of PRO data should be valued, especially in this indication; however, the publication of PRO data along with other critical trial endpoints was not seen in many of the initial trial reports. The collection of PRO data should result in routine, timely, and appropriate reporting as part of the trial outcome publication, to allow for a thorough assessment of investigational clinically relevant treatment effects. If the primary trial publication does not include the PRO results, there should be a reference or acknowledgment to the impending PRO publication. Future research in this field may evaluate the reasons why PROs are not implemented more often in clinical trials and what causal factors have influenced the under-reporting of PRO data in trial publications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal