Background:
Thrombotic microangiopathic anemia (TMA) is a hematological emergency that requires prompt review of a peripheral blood smear for the presence of schistocytes. Within our institution, we had concern for lack of consistency in identifying schistocytes, lack of consistency in reporting methods, possible variation in schistocyte quantitation due to microscope differences, and the threshold for which our laboratory had been reporting increased schistocytes. The objective of our quality improvement project was to implement published practice standards for morphological identification, quantitation, and reporting of schistocytes across different groups at the University of Cincinnati Medical Center (UCMC).
Methods:
The International Council for Standardization in Haematology (ICSH) recommendations for the identification, diagnostic value, and quantitation of schistocytes (Zini et. al. International Journal of Laboratory Hematology 2012) were reviewed prior to designing this project.
We next conducted a survey of groups that were reviewing peripheral blood smears for schistocytes on a routine basis: medical technologists (n=9), pathology residents (n=10) and hematology-oncology fellows (n=13). The survey included questions about schistocytes, including desire for standardization and normal reference values, desire for pathologist instruction, and reporting patterns. One question included 8 images of various red cell morphologies, and participants were asked to select ones they would classify as schistocytes.
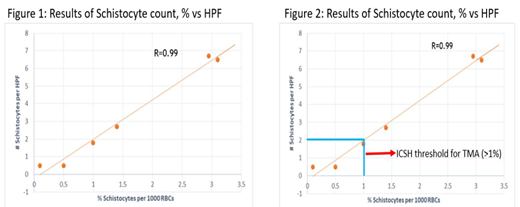
The microscopes were compared for objective and field diameter measurements. Six (6) peripheral blood smears with previously reported schistocytes were re-reviewed. Schistocytes were identified per ICSH guidelines and counted as a percentage (%) of 1000 total red blood cells using a Miller optical disc and also as an average number per field for a total of 10 high power fields. The results were plotted on a linear X-Y axis graph (Fig 1) and compared to the ICSH guidelines (Fig 2) and the policy for reporting schistocytes in our laboratory.
Results:
Survey results showed that the majority of each group desired standardization, normal reference values, and pathologist instruction. For reporting of schistocytes, residents answered present/absent (50%) or average per high power field (HPF) (50%), whereas 92% of fellows answered average per HPF. No participants reported a percentage of 1000 red blood cells, the current ICSH recommendation.
For the morphological identification, 50% of residents, 62% of fellows and 67% of technologists correctly identified keratocytes as schistocytes. Fifteen (15%) of fellows misidentified bite cells as schistocytes, whereas one fellow (8%) and one technologist (11%) misidentified acanthocytes as schistocytes. Only 70% of technologists correctly identified helmet cells as schistocytes, whereas all residents and fellows chose them correctly. Almost all participants failed to recognize microspherocytes as schistocytes.
The microscopes all showed the same objective and field diameter measurements. The schistocyte percentage plotted versus the number of schistocytes per HPF showed a 0.99% correlation co-efficient (R=0.99%) (Fig 1). The results were compared to the ICSH threshold of 1%, above which the ICSH reports is a robust morphologic indicator for the diagnosis of TMA (Fig 2), and to the current reporting policy at UCMC. Two (2) schistocytes per HPF correlated with 1% schistocytes on the linear plot. At UCMC, policy had been to report 2-8 schistocytes per HPF as present and >8 per HPF as increased. These findings indicated that the threshold for reporting increased schistocytes should be lowered from >8 per HPF to >2 per HPF.
The above data were reviewed with each survey group. A process was also initiated to change the laboratory schistocyte reporting policy.
Conclusion:
All survey groups needed and desired education on schistocyte identification and reporting per ICSH guidelines. All microscopes showed the same measurements and were therefore expected to produce the same quantitation results. Schistocyte percentage correlated with the number of schistocytes per HPF. By implementing the ICSH guidelines, we aimed to decrease inter-observer bias and to standardize the quantitation and reporting of schistocytes at UCMC, thereby assisting in timely and accurate diagnosis of thrombotic microangiopathic anemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal