Introduction
The overall impact of morbidity related to sickle cell disease (SCD) is enormous due to decreased quality of life, high health care utilization and immense financial strain on the patients and health care system. Patients with SCD have also been found have high hospital readmission rates compared to other medical conditions, further leading to increased health care burden. The objective of this study was to explore the common reasons, healthcare utilization and identify modifiable factors associated with 30-day readmission in patients with SCD using the most recently available national data in the United States.
Methods
Cohort selection. 2016 Nationwide Readmission Database (NRD) from the Healthcare Cost and Utilization Project (HCUP) by the Agency for Healthcare Research and Quality (AHRQ) was queried for analysis. NRD captures discharge data from 22 states, representing about 50% of all hospitalizations in the United States. National estimates can be produced by using sampling weights provided by the NRD. Patients with SCD were identified by using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis code D57. Patients younger than 18 years were excluded. Readmission was defined as any admission within 30 days of index hospitalization discharge.
Statistical Analysis. Sampling weights were used throughout all calculations, facilitating appropriate national projections. Percentages in all figures reflect national estimates. Chi-square test and Student's t-test were used for univariate analysis. Multivariable logistic regression analysis was done to determine independent predictors of 30-day readmission in patients with SCD. Data analyses was performed using SAS v9.4 (SAS Institute, Cary, NC).
Results
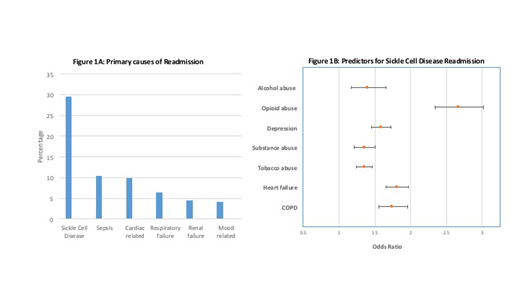
In a total of 83,692 hospitalizations for SCD in 2016, 15,880 (18.9%) had at least one 30-day readmission and 40% of the readmissions occurred within the first two weeks of discharge. The most common reason for 30-day readmission was due to complications of SCD (29.8%) with sickle-cell pain crisis (18.4%) being the most frequent one. The other common causes for readmission were sepsis (10.3%), cardiac related (9.7%), respiratory failure (6.2%), renal failure (4.3%) and mood related (4.04%). Female sex (P<0.001), younger age (p<0.01) and patients with public insurance (P <.001) were more likely to be readmitted. Multivariable logistic regression analysis showed age 31-45 years (OR 1.28, 95% CI 1.16 - 1.40, P<0.01), alcohol abuse (OR 1.39, 95% CI 1.17 - 1.66, P<0.001), opioid abuse (OR 2.66, 95% CI 2.34 - 3.02, P<0.0001), depression (OR: 1.59, 95% CI 1.45 - 1.73, P<0.01), substance abuse (OR: 1.35, 95% CI 1.21 -1.50, P<0.001), tobacco use (OR: 1.35, 95% CI 1.24 - 1.46, P<0.01), heart failure (OR: 1.81, 95% CI 1.66 - 1.97, P<0.002), COPD (OR: 1.74, 95% CI 1.55 - 1.96, P<0.03) were significantly associated with 30-day readmission while adjusting other co-morbidities. The mean cost of readmission was an additional $39,259 (±182).
Conclusion
This study showed that the 30-day readmission rate in patients with SCD in 2016 has decreased to less than 20% compared to previously published rates (31.9%, Elixhauser A, 2013). While this decrease in readmission rate is encouraging, further studies are needed to investigate the reasons for this trend. Several modifiable risk factors were identified in this study such as alcohol, tobacco, opioid, substance abuse and depression which can be addressed to potentially bring down the readmission rate further and improve patient care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal