Introduction:
Current expert recommendations recommend double therapy (DT) over triple therapy (TT) in atrial fibrillation patients post percutaneous coronary intervention (PCI) to prevent the incidence of stroke. Though previous studies have focused on DT (oral anticoagulant [OAC] + P2Y12 inhibitor (including clopidogrel, ticagrelor and prasugrel)) versus TT (OAC + P2Y12 inhibitor and aspirin) strategy, no study assessed which OAC was more effective in the prevention of cardiovascular events and stroke. To this end we performed a systematic review and meta-analysis to assess whether non-vitamin K oral anticoagulants (NOAC) based DT strategy is comparable with vitamin K antagonist-based TT in patients with AF after PCI.
Methods:
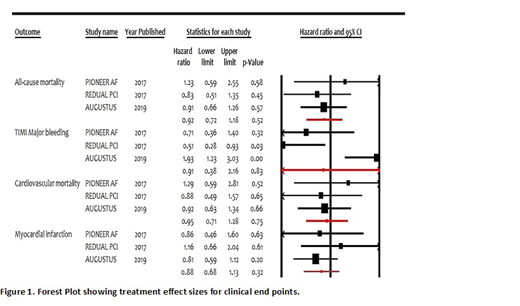
Embase, Ovid, Pubmed and Scopus were extensively searched for only phase 2 and 3 clinical trials comparing NOAC based DT with VKA based TT from inception of these databases till June 2019 by two independent reviewers. The endpoints were all-cause mortality, Thrombolysis in Myocardial Infarction (TIMI) major bleeding, cardiovascular mortality and myocardial infarction. Cochrane Collaboration's tool was used for risk of bias assessment. Statistical heterogeneity was quantified using I2 statistics. Publication bias was assessed with Eggers regression test. Estimates were reported as hazard ratios (HR) with 95% confidence intervals (CI) using random effect model. Rivaroxaban 15 mg once daily dose from PIONEER-AF was included. From REDUAL-PCI trial we included dabigatran 110 mg BID and 150 mg BID doses. AUGUSTUS trial used 5 mg BID or 2.5 mg BID dosing of apixaban.
Results:
402 trials were retrieved in the initial search which were analyzed according to PRISMA (Preferred Reporting Items for Systematic review and Meta-Analyses) guidelines. Three trials (Augustus, PIONEER AF-PCI and RE-DUAL PCI) were extracted that met the inclusion criteria and included in the final analysis evaluating 8754 patients. Twenty seven percent were females. Mean age was 71 years. PCI was done for acute coronary syndrome in 44% of the patients. Mean calculated CHA2DS2-VASc was 4 which qualifies the use of oral anticoagulants. Only PIONEER AF-PCI and RE-DUAL PCI trials described the type of stent used for PCI. Drug eluting stents were used in 71% of the patients. There was no evidence of publication bias in our analysis (P=.78). The studies overall had low risk of bias. Our analysis showed no statistically significant difference in usage of NOAC + P2Y12 inhibitor compared to triple therapy consisting vitamin K antagonist in regards to all-cause mortality, (HR 0.92, 95% CI 0.72-1.18, P=.52), thrombolysis in myocardial infarction (TIMI) major bleeding (HR 0.91, 95% CI 0.38-2.16, P=.83), cardiovascular mortality (HR 0.95, 95% CI 0.71-1.28, P=.75), stroke (HR 1.07, 95% CI 0.67-1.71, P=.78),stent thrombosis (HR 0.72, 95% CI 0.42-1.23, P=0.23) and myocardial infarction (HR 0.88, 95% CI 0.68-1.13, P=.32).
Conclusion:
We conclude that there is no difference between the usage of NOAC including rivaroxaban, dabigatran and apixaban in dual regimen vs triple therapy with VKA (warfarin). However, some limitations need to be considered such as heterogeneity across patients in terms of indication for PCI (elective vs emergency), choice of P2Y12 inhibitor (clopidogrel vs ticagrelor vs prasugrel), mean duration of therapy (range 6-12 months) and mean length of follow-up (range 6-14 months). In future clinical practice, post-PCI antithrombotic regimens in AF will likely consist of a single P2Y12 inhibitor plus NOAC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal