Background:
Anemia has an estimated prevalence of 5.6% in the overall United States population. In patients undergoing cardiac surgery, as many as 16-54% of patients are estimated to have anemia. Common causes of anemia in the perioperative setting include iatrogenic anemia due to blood draws and lab tests, iron deficiency anemia, and anemia of chronic disease. Studies show that patients with pre-operative anemia undergoing coronary artery bypass surgery have increased lengths of stay in the hospital and higher 30-day mortality rates post-operatively compared to non-anemic patients. The use of transfusions to address blood loss anemia is quite common, as approximately 50% of all patients undergoing cardiac surgery receive blood. In addition to common risks associated with transfusions, studies also note that in cardiac surgery patients, there is an increased risk of infection associated with receiving blood products.
To address the issue of pre-operative anemia, we developed an Anemia Clinic to help optimize patients scheduled to undergo non-emergent cardiac surgery. Patients meet with a multidisciplinary team and interventions including lifestyle modifications, erythropoietin-stimulating agents, and intravenous iron are utilized to help patients reach target hemoglobin values, per surgeon preference. The length of treatment through the Clinic is individualized for each patient based on the risk-benefit analysis of delaying surgery and the amount of time available between evaluation by the clinic and the anticipated date of the procedure. To date, 21 patients have been evaluated in the clinic and have successfully undergone cardiac surgery.
Methods:
Patients included in our study were those who were assessed through the Anemia Clinic following referral from their cardiac surgeons. Baseline characteristics, including lifestyle choices, tobacco use, exercise routines, and pre-operative complete blood count, basic metabolic panel, iron studies, and when possible, erythropoietin levels, were obtained. Patients then were evaluated by a multidisciplinary team comprised of physicians, nurses, social workers, and dietitians. Those who do not accept blood products also met with Transfuse-Free Medicine Care Coordinators. Prior to surgery, we measured hemoglobin values. Following surgery, we assessed two primary endpoints, namely post-operative transfusion rates and 30-day readmission rates.
Results:
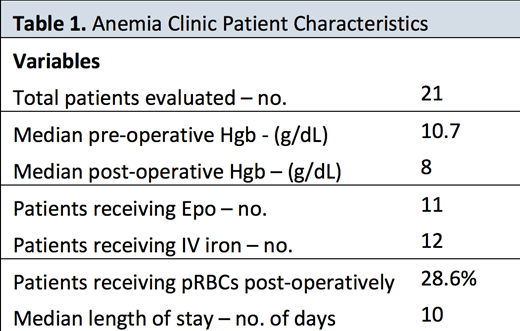
In total, 21 patients have been evaluated in our Anemia Clinic. We report that 6 patients received post-operative blood transfusions (28.6%). Furthermore, we report zero 30-day readmissions. Other data are presented in Table 1.
Conclusion:
Through the use of a multifaceted approach, hemoglobin optimization prior to cardiac surgery results in improved outcomes. Blood transfusions were required in only 28.6% of patients, compared to national averages of approximately 50%. Furthermore, we report zero hospital readmissions in 30 days, as compared to state-average readmission rates following cardiac surgery of 11.7%. Overall, our approach to hemoglobin optimization appears to improve outcomes for patients undergoing cardiac surgery.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal