Introduction: Adults living with sickle cell disease (SCD) have high utilization of emergency departments (ED) and hospitals, and utilization typically is skewed with a subgroup with very high utilization. We sought to promote a shift from ED/hospital utilization to ambulatory care (Amb) services in our state through ED/hospital visit-prompted communication with ED/hospital and Amb practitioners.
Methods: The Community Health Network of Connecticut, Inc. (CHNCT) is the medical administrative services organization (contractor) for the physical health benefit of the state's Medicaid Program, HUSKY Health. Among HUSKY members ages 16 years and older (16+) with Medicaid-only insurance and with at least one Medicaid payment claim with a primary or secondary ICD-9/ICD-10 diagnosis of sickle cell disease from Feb 28, 2016 thru Feb 25, 2017, we identified high ED/hospital utilizing members.
CHNCT monitored high utilizing 16+ member ED/hospital visits in real time using admission, discharge, and transfer data, and provided practitioner team members with individual member utilization data (mUD) to be shared via telephone contact with ED/hospital and Amb practitioners when 16+ members visited an ED or were hospitalized. Shared mUD included numbers of ED/hospital visits, names of ED/hospital facilities visited, and information about Amb services visits. ED/hospital practitioners were encouraged to advise members to seek regular care from one of the state's hospital-based SCD programs or other practitioners.
No formal hypotheses were declared for testing for statistical significance. Differences in utilization were compared with the Mann-Whitney U test.
Results: We identified 705 16+ members living with SCD. In phase 1, high utilizing members (HUM1) were defined as individuals with 12+ ED visits or 8+ hospital visits in the reference year. We identified 45 (6%) HUM1 who accounted for approximately half of all 16+ member ED visits [1364 (56%) of 2436] and hospital visits [368 (47%) of 788]. Among HUM1, the distribution of visits was highly skewed with individual HUM1 accounting for up to 184 ED and up to 27 hospital visits. HUM1 used up to 27 facilities, some out-of-state. In phase 2, we identified an additional 47 members (HUM2) with 6+ ED visits or 4+ hospital visits in the reference year.
From Aug 2017 to Jun 2019, CHNCT notified clinical team members of 504 ED/hospital visits involving 51 HUM, and clinical team members shared mUD with practitioners on 342 (68%) occasions. For data analysis, the HUM1 pre-information sharing period was defined as 1/1/16 thru 11/9/16; the post-information sharing period was defined as 7/11/16 thru 7/10/17. For HUM2, pre- 6/6/17 thru 6/5/18, and post- 6/6/18 thru 12/13/18. As the duration of time periods differed, data were expressed as visits (or dollars) per year.
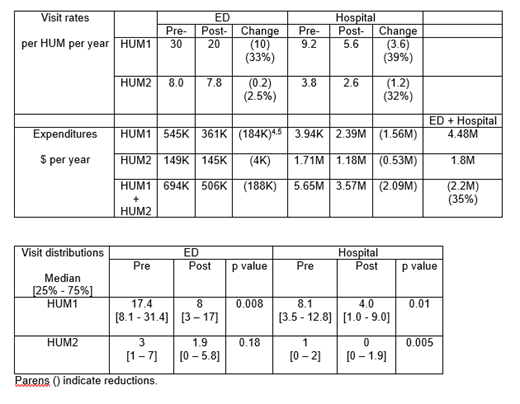
ED visit rates fell by one third for HUM1 (33%), but were little changed for HUM2 (see Table 1). Hospitalization rates fell by about one third for both HUM1 (39%) and HUM2 (32%). P values for changes in ED visit rates for HUM1 and HUM2 and in hospitalization rates for HUM2 ranged from 0.005 to 0.01. Medicaid ED and hospital expenditures per year fell more than one third (35%), or about $2.2M.
Conclusions: Six percent of CT Medicaid members 16 years and older living with SCD accounted for approximately half of all those members ED and hospital utilization. Visit-prompted sharing of utilization data of these high utilizing members with ED, hospital, and Amb practitioners coupled with a recommendation to advise these members to seek regular Amb services led to decreases in ED visits, hospitalizations, and total expenditures by about one third. The same intervention applied to a cohort of the next highest utilizing members resulted in a similar change in hospitalizations but minimal change in ED visits. Medicaid expenditures for ED visits and hospitalizations for the groups combined fell by about one third, or $2.2 million per year. It will be important to ascertain whether information sharing changed utilization of Amb services.
This quality improvement project is HIPAA compliant; no institutional review board approval was required.
Roberts:Community Health Network of Connecticut: Consultancy; Truven Health Analytics: Consultancy. Andemariam:Emmaus: Membership on an entity's Board of Directors or advisory committees; New Health Sciences: Membership on an entity's Board of Directors or advisory committees; Sanofi Genzyme: Membership on an entity's Board of Directors or advisory committees; Terumo BCT: Membership on an entity's Board of Directors or advisory committees; Global Blood Therapeutics: Other: DSMB Member; Imara: Research Funding; Cyclerion: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; NovoNordisk: Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees; Community Health Network of Connecticut: Consultancy. Latham:Community Health Network of Connecticut: Employment. Cyr:Community Health Network of Connecticut: Employment. Magras:Community Health Network of Connecticut: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal